A Reason to Cry Uncontrollably
Danny Glover did a “public awareness” ad for pseudobulbar affect (PBA) in 2015. In the ad, he said if you have PBA, choosing to laugh or cry may not be your decision. The ad went on to note PBA is a neurological, not psychological condition that is treatable; by Avanir’s Nuedexta. You were given information to “get the facts” about PBA. But one of the facts you wouldn’t get is that almost half of Nuedexta claims filed with Medicare in 2015 “were filed by doctors who had received perks (financial or otherwise) from Avanir.”
The above quote was from an article on Nuedexta from the website Nursing Home Abuse Center that highlighted a CNN investigation into Avanir and Nuedexta. While experts say that PBA effects less than 5 % of elderly patients, CNN found that “more than half of all Nuedexta pills manufactured since 2012 have gone to nursing homes.” While Avanir claims in its ads that PBS can occur with patients having Alzheimer’s or dementia, it admits Nuedexta has not been extensively studied among elderly patients.
One study among Alzheimer’s patients found those taking Nuedexta were twice as likely to suffer a fall, not something you want to see with the elderly. “Fall risk has been a huge concern among Nuedexta users since 2013 when nursing home inspectors first started questioning use of the drug in dozens of nursing homes across the United States.” The CNN investigation found over 80 cases through 19 states where nursing homes were cited for inappropriate use and monitoring of Nuedexta. Sometimes it was given to patients without a formal prescription or doctor approval. “Many of the cases were based on the fact that patients exhibited no signs of PBA.”
The original CNN investigation reported in October of 2017 stirred up concerns and significant interest in Avanir and its marketing tactics with Nuedexta. The same two reporters have written a series of articles on CNN since then noting how Los Angeles opened an investigation into Avanir following the CNN report; how a leading advocacy group for Alzheimer’s stopped accepting contributions from Avanir after the report; and that the US government warned insurance companies to look for suspicious prescriptions of Nuedexta. And there were several doctors with problem records, at least three had criminal convictions for illegal prescribing, promoting Nuedexta.
The Los Angeles City Attorney confirmed his office was seeking information and tips from the public to help assess whether state or federal laws were violated in the sale, marketing or prescribing of Nuedexta. The people receiving Nuedexta are vulnerable and rely on others to make decisions for them. “If there is a possibility they are being administered a medication not because it is in their best interest, but because it is in the financial interest of, say, the drug manufacturer, then it is important for us to intervene.” He said he would look for potential illegal activity including kickbacks to doctors and off-label marketing of Nuedexta, that is suggesting it as a treatment for any purpose not approved by the federal government.
This would include using it as a “chemical restraint” to sedate or control behavior problems. “State regulators … have found cases of doctors inappropriately diagnosing nursing home residents with PBA to justify using Nuedexta to treat patients whose confusion, agitation and unruly behavior make them difficult to manage.” In one LA nursing home, regulators found that 28% of its residents (46 of 162) had been placed on Nuedexta. A facility psychiatrist, a paid speaker for Avanir, had given a talk about the drug to employees.
At another facility, also in Southern California, an employee admitted to inspectors that a resident had been given a diagnosis of PBA to “somehow justify the use” of Nuedexta, even though its intended purpose was to control the resident’s “mood disturbances” and yelling out.
In order to line up prescriptions, sales people identified doctors, nurses and pharmacists who could be advocates for the drug. Then they worked closely with these advocates to identify potential patients. One salesperson worked with a doctor’s office manager to pull patient’s charts and identify those who should be screened for PBA. “CNN’s investigation also found that the sales force coached doctors and facility employees on how to fight for Medicare coverage of the drug if it was initially refused.”
Another CNN article noted that after the original CNN article on Avanir and Nuedexta, the Alzheimer’s Association said it would not accept any further funding from Avanir, pending the results of the LA City Attorney. Avanir gave the group almost $200,000 in 2017. In a statement, the association said: “We are committed to people living with the disease, and we encourage vigorous review and oversight of companies and prescribers to ensure best practices are followed for those impacted by Alzheimer’s disease.” It added the contribution by Avanir was only .056% of its annual revenue.
Another nonprofit, the Alzheimer’s Foundation of America, said it received $60,000 from Avanir in 2016-2017. The organization declined to comment on the findings of CNN’s report, adding that it stood by its educational programs and that Nuedexta is not mentioned in Avanir presentations. Nuedexta is the only FDA approved treatment for PBA. One of its medical advisory board members said the AFA’s Educational Conferences provide caregivers an opportunity to understand and recognize PBA, “which afflicts a certain percentage of those with dementia.”
“Between 2013 and 2016, he received nearly $50,000 from Avanir, in the form of consulting and royalty or licensing fees, as well as travel and meals, according to government data.” He was also the lead author on the Avanir-funded study on Nuedexta that found patients on Nuedexta were more than twice as likely to fall (8.6% versus 3.9%) than those on a placebo. A research professor who studies the marketing tactics of pharmaceutical companies said Avanir’s ties with nonprofit dementia advocacy groups was “deeply troubling” and a conflict of interest. This was a particular concern for him “because Nuedexta has not been approved specifically for Alzheimer’s or dementia.
Between 2013 and 2016 Avanir Pharmaceuticals paid almost 500 doctors to speak or consult on Nuedexta. After reviewing the top prescribers of Nuedexta, CNN noted 12 who had been disciplined by state medical boards. Former Avanir employees said the company’s speaker program sought out doctors and pharmacists to present the drug to medical colleagues and nursing home employees. “Avanir and its parent company, Otsuka, paid doctors nearly $14 million for Nuedexta-related consulting, promotional speaking and other services.” In effect, these doctors are being used as a sales force, according to Michel Santoro, an expert in pharmaceutical industry ethics at Santa Clara University.
Many of the doctors with medical board issues identified by CNN involved other medications such as opioids. But one case centered on the use of Nuedexta. An Oregon doctor had already been banned by the state board from providing mental health treatment to inmates. Then he was summoned for his treatment of four nursing home patients. For one of his patients he attempted to prescribe Nuedexta “when there was no support for a PBA diagnosis.” The others were cases of inappropriately prescribing medications, changing doses or discontinuing drugs without explanation. Despite all these allegations, he was being paid by Avanir to speak publically about Nuedexta.
Then in June of 2018 CNN reported they had received documents through a public records request that indicated there have been complaints filed with the FDA about Avanir’s marketing and advertising dating back to 2012. BlueCross BlueShield of Arizona said Avanir was misrepresenting Nuedexta as “safe and effective” in populations it had not been approved for or adequately studied. “We believe that the manufacturer appears to be marketing Nuedexta far beyond the scope of the clinical evidence.” An individual complaint in 2016 said they had overheard a salesperson promote the drug for unapproved uses. “Specifically they are targeting [sic] residents with Dementia with Behavioral Disturbances.”
In March of 2018 CMS (Centers for Medicare & Medicaid Services) issued a memo asking Medicare insurance providers to monitor prescriptions for Nuedexta in order to ensure it was being appropriately given to patients. The memo reminded plan sponsors that Nuedexta was only approved to treat PBA and that insurers were legally required to ensure it was only being used for medically accepted uses. The agency said the memo was provided to “inform plan sponsors about increases in utilization that may not be readily discerned or may relate to potential fraud.”
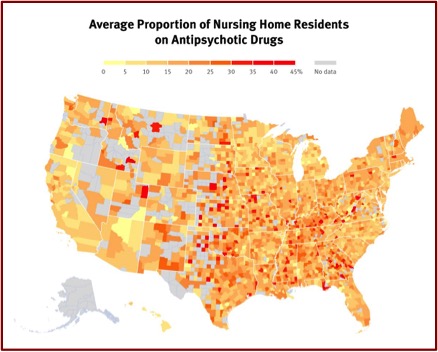
Sadly, Avanir seems to have placed profits ahead of ethical medical care with the elderly. They have encouraged the use of Nuedexta in nursing facilities as a kind of chemical restraint. This seems to have partly occurred in response to the FDA tightening regulations on the use of antipsychotics for the same reason. There is a reason to cry uncontrollably, but it’s for how Neudexta has been mis-marketed and mis-prescribed. For more on Nuedexta and the use of antipsychotics in nursing homes, see “Conjuring Diagnoses for the Elderly” and “Nursing Homes Want Docile.”