Double Whammy of Teens Vaping Marijuana
The FDA recently announced there is a “growing epidemic of youth e-cigarette use” and held a hearing on December 5th to discuss efforts to eliminate teen e-cigarette use. Since 2014, the most commonly used method of consuming tobacco products among teens has been vaping—“used by 1.73 million (11.7 percent) high school students and 390,000 (3.3 percent) middle school students in 2017.” FDA Commissioner Scott Gottlieb expressed concern that a large pool of nicotine users is being created among school-age children. But that isn’t the only substance teens are smoking more. In JAMA Pediatrics a research letter said nearly one-third of middle and high school students are vaping marijuana.
USA Today reported the researchers found 8.9% of those surveyed said they had smoked marijuana in e-cigarettes. “Among those who reported vaping, nearly 1 in 3 high school students and about 1 in 4 middle school students reported using cannabis in the devices.” Unless the manufacturers can prove they are trying to stop children and teens from using e-cigarettes, the FDA will stop the sales of flavored ones. “We’re going to have to take action.”
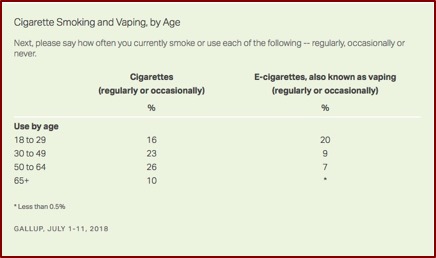
Gallup also reported that vaping is more prevalent among Americans who were under 30. While 9% of all Americans said they regularly or occasionally vape, 20% of those who were between the ages of 18 to 29 do so. This compared to 8% among those who were 30 to 64 years of age; and less than 5% among those 65 and over. See the following table.
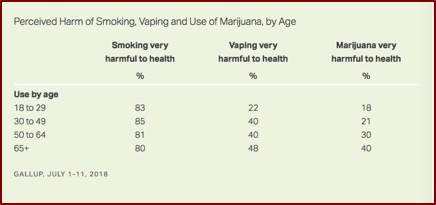
 Young people were less likely than those over 30 to believe vaping was risky; somewhat parallel to their views on marijuana. Twenty-two percent of those under 30 believe vaping was “very harmful” to your health, compared to at least 40% for every other age group. Notice how at the same time young people’s views about the health effects of traditional smoking was no different than older age groups’ views. See the following table.
Young people were less likely than those over 30 to believe vaping was risky; somewhat parallel to their views on marijuana. Twenty-two percent of those under 30 believe vaping was “very harmful” to your health, compared to at least 40% for every other age group. Notice how at the same time young people’s views about the health effects of traditional smoking was no different than older age groups’ views. See the following table.
 There are several things that make vaping marijuana appealing to teens, according to Bonnie Halpern-Fisher. Vaping has less of an odor than smoking. And marijuana is increasingly easier to obtain, as it is legal in ten states for adults. Helpern-Fisher also expressed concern over the number of youth vaping marijuana. “You’re basically using it in a very strong form.” Teens face a special risk because their brains are still developing: “Youth are at a very vulnerable time.” See “Priming Young Adults with Vaping” for more on marijuana use and vaping among teens.
There are several things that make vaping marijuana appealing to teens, according to Bonnie Halpern-Fisher. Vaping has less of an odor than smoking. And marijuana is increasingly easier to obtain, as it is legal in ten states for adults. Helpern-Fisher also expressed concern over the number of youth vaping marijuana. “You’re basically using it in a very strong form.” Teens face a special risk because their brains are still developing: “Youth are at a very vulnerable time.” See “Priming Young Adults with Vaping” for more on marijuana use and vaping among teens.
A small study in JAMA Network Open found that vaporized cannabis resulted in “significantly greater subjective drug effects, cognitive and psychomotor impairments, higher blood THC concentrations than the same doses of smoked cannabis.” They speculated the procedures in former studies enabled users to titrate their THC dose, while the current study required participants to self-administer a fixed amount of cannabis. “Therefore, holding THC dose constant, vaporizers appear to be a more efficient cannabis and THC delivery method, likely because with traditional smoked preparations, more THC is lost as a result of pyrolysis (combustion) and/or sidestream smoke.” The researchers concluded:
In this study, participants experienced dose-orderly increases in subjective drug effects, cognitive and psychomotor impairment, acute cardiovascular effects, and blood THC concentrations following inhalation of smoked and vaporized cannabis. Notably, vaporized cannabis produced greater changes in study outcomes relative to smoked cannabis. As the legal cannabis marketplace continues to expand, future studies should further explore the effects of vaporizers and other novel methods for cannabis administration in users with different degrees of experience with cannabis, as the pharmacokinetic and pharmacodynamic profiles will likely differ substantially across products and users.
However, the effects on cognitive functioning could be temporary in some cases. A meta-analysis by Scott et al., published in JAMA Psychiatry, found there was a “small but significant overall effect size for reduced cognitive functioning in adolescents and young adults” reporting frequent cannabis use. The studies requiring abstinence longer than 72 hours had a small, nonsignificant effect size. The researchers speculated that reported deficits could reflect residual effects from acute use or withdrawal.
Nevertheless, Gruber et al. said in “The Grass Might be Greener” there is a large body of evidence suggesting marijuana use was related to cognitive decrements, including deficits in verbal memory, attention and executive function. And while these deficits were found in adult marijuana users, they were more prominent in adolescent users, who were in the midst of neurodevelopment. The deficits have also been linked to changes in brain structure and function. “Similar to studies of cognitive performance and brain structure, fMRI studies have revealed that earlier onset of MJ use is related to altered patterns of brain activation during tasks requiring cognitive control and inhibition.”
It seems that this poorer cognitive performance was due to the effects of THC (Δ9-tetrahydrocannabinol), while CBD (cannabidiol) has been shown to improve cognitive function. “In general, studies suggest that THC and CBD have opposite effects on cognition-related brain activation.” So they hypothesized that after 3 months of medical marijuana treatment, patients would demonstrate improved task performance and these changes would coincide with changes in brain activation patterns measured by fMRI.
Following 3 months of MMJ treatment, patients exhibited improved task performance and related alterations in frontal brain activation patterns during the completion of the MSIT, a measure of executive function and cognitive control, relative to pre-MMJ treatment. Within the cingulate cortex (CC), patients did not exhibit any significant pre-treatment activation during the Interference condition of the MSIT; however, after 3 months of treatment, robust activation was noted within this region. In fact, the magnitude of activation significantly increased over the course of treatment such that post-treatment activation patterns appeared more similar to that of healthy controls observed in previous studies. Activation within the frontal ROI was also notably increased following 3 months of MMJ treatment relative to pre-MMJ treatment. Taken together, these changes may be reflective of a potential “normalization” of brain function following 3 months of MMJ use.
There was also improved task performance and self-reported improvements in mood and quality of life, as well as reduced sleep disturbance and lower motor impulsivity. “It is possible that improvements in symptomatology (i.e., relief of symptoms, improved mood/sleep) are directly related to observed improvements in cognitive function and alterations in brain activation.”
While findings in this study show improvements in cognitive task performance, previous studies entirely focused on recreational (THC) marijuana users have reported decrements in cognitive performance. Among the factors that may account for this difference, Gruber et al. noted the majority of prior studies of recreational marijuana use included adolescent and young adult populations. Studies have overwhelmingly demonstrated that early onset of recreational marijuana use was related to poorer task performance and changes in brain function. Given that participants in their study were well-beyond the critical stages of neurodevelopment (mean age=50.64), “They are less likely to be vulnerable to the adverse neural effects of THC.”
The dangers then seem to be from recreational marijuana use—in other words from strains with higher THC and lower CBD levels. Early onset of recreational marijuana use also increases the adverse effects of cognitive decrements. When these factors are added to the FDA’s concern with the “growing epidemic of youth e-cigarette use,” there seems to be a double whammy to finding that nearly 1 in 3 high school students are vaping marijuana. They are in danger from increased exposure to nicotine and marijuana.


