To Reschedule or “Deschedule” Marijuana?

The DOJ and DEA published proposed rules in the U.S. Federal Register to reschedule marijuana from Schedule I to Schedule III. The DOJ was also soliciting comments on the proposal on or before July 22, 2024. Forbes said the proposal initiates a 62-day public comment period, a necessary step in the federal rulemaking process. This action was taken after the Department of Health and Human Services (HHS) recommended the reclassification, stating that marijuana had a currently accepted medical use. But the action won’t legalize marijuana for adult use, which would require it to be completely “descheduled” by the Controlled Substances Act (CSA).
The DEA’s notice indicated that if marijuana is reclassified to Schedule III, the regulatory controls for Schedule III substances, when appropriate, would apply. These controls would include existing marijuana-specific requirements and any additional ones necessary to meet U.S. treaty obligations. The major change for the cannabis industry with the reclassification of marijuana to Schedule III, would allow marijuana businesses to take certain deductions on their federal tax returns.
The manufacture, distribution, dispensing, and possession of marijuana would still be subject to the criminal prohibitions of the CSA. Drugs containing substances defined as “marijuana” under the CSA would also remain subject to the prohibitions in the Federal Food, Drug, and Cosmetic Act.
Writing for Harvard Law, Victoria Litman pointed out that once comments are received, the DEA will review all evidence and generally respond to the comments when publishing the final rule. After publication, the DEA’s final rule will not go into effect for 30 days, during which time parties who submitted comments, and can demonstrate they have a standing, could challenge the final rule in court. SAM, Smart Approaches to Marijuana, is already soliciting funds for their “Rescheduling Legal Defense Fund.”
Litman thought there are two primary issues that will be challenged. First is the impact of rescheduling on U.S. adherence to United Nations treaty obligations. Second, was the way HHS determined that marijuana has a currently accepted medical use (CAMU). She pointed out how rescheduling would not resolve all the challenges faced by legal state marijuana businesses and wouldn’t necessarily make research easier.
Additionally, U.S. Senators Elizabeth Warren and John Fetterman have sent a letter to the DOJ and DEA urging that marijuana be descheduled altogether from the CSA. In their letter they said the case for removing marijuana from Schedule I was overwhelming. However, they thought the DEA should remove cannabis from the CSA altogether:
Although HHS recommended rescheduling, its analysis could support a decision to deschedule— particularly its emphasis on the fact that marijuana has less adverse outcomes (including less potential of an overdose) and less potential of abuse than substances that are descheduled (alcohol) or scheduled below Schedule III (such as benzodiazepines).
While there would be important policy benefits including the first federal acknowledgement of marijuana’s medical uses, “it would not automatically permit marijuana to be used as a medicine.” Marijuana as an approved medicine would still need to have FDA drug approval, DEA registration for manufacturers, “and compliance with prescription regulations in order to be legally prescribed under federal law.” Furthermore, the criminal penalties for marijuana would continue as long as marijuana remained in the CSA. They concluded the DEA had never kept a drug in Schedule I after HHS recommended removing it.
A History of the FDA and Drug Regulation in the U.S. said the original Food and Drug Act was passed in 1906. The Federal Food, Drug and Cometic Act of 1938 required new drugs demonstrate their safety before selling them. The Controlled Substances Act was part of the Comprehensive Drug Abuse Prevention Act of 1970. It combined existing federal drug laws and expanded their scope, including federal law enforcement pertaining to controlled substances. It is the primary legislation for drug control in the U.S., and has been amended several times. Warren and Fetterman said:
It is imperative that the DEA remove marijuana from Schedule I as several members of Congress and state attorneys general have urged. The DEA should do so promptly; its past record of taking years to resolve rescheduling petitions should not be repeated here. Furthermore, the DEA and HHS should be fully transparent about the evidence relied upon in the course of their review processes. The Biden Administration has a window of opportunity to deschedule marijuana that has not existed in decades and should reach the right conclusion— consistent with the clear scientific and public health rationale for removing marijuana from Schedule I, and with the imperative to relieve the burden of current federal marijuana policy on ordinary people and small businesses.
Senators Warren and Fetterman don’t seem to think the HHS recommendation to reclassify marijuana from Schedule I to Schedule III goes far enough. They want to see marijuana removed entirely from the CSA. They also think the DEA should make its decision quickly, and not take time to resolve problems raised by the rescheduling petitions, as it has in the past. This raises the question, what’s the rush?
John Fetterman has made the legalization of recreational marijuana part of his political platform from the time he was the Lieutenant Governor of Pennsylvania. He did a Statewide Cannabis Listening Tour in 2019. He also called for PA to go “full Colorado,” meaning approve recreational marijuana. See these articles and others on Fetterman’s endorsement of legalizing recreational marijuana: “From the Frying Pan Into the Fire with Recreational Marijuana In PA” and “Should Pennsylvania Go ‘Full Colorado’ with Marijuana?” Part 1 and Part 2.
Marijuana Moment observed that the director of the Office of National Drug Control Policy (ONDCP) said rescheduling was “going to be really important to remove barriers to critical research and perhaps drug development, and it could also lead to more research into the benefits of medical marijuana.” The historic nature of the proposed actions “Cannot be minimized,” he said. Yet Marijuana Moment thought he overstated what this reform would accomplish. The FDA hasn’t typically approved botanical substances like marijuana as prescription drugs. According to the Congressional Research Service, (CRS) further action from the FDA is needed before marijuana products can become available by prescription.
Without a doubt this is a political issue in a contentious presidential election year, but it’s also a business concern. Flowhub said the cannabis industry was expected to reach $40 billion in 2024, adding $115.2 billion to the economy. There are currently 440,445 full-time equivalent positions supported by legal cannabis. The anticipated financial windfall to the cannabis industry may lead them to minimize or ignore some of the potential repercussions of either rescheduling or descheduling marijuana. Given the “historic nature” with either decision, shouldn’t the DEA carefully consider the impact of the proposed actions?
STAT News said the public health use of marijuana has surpassed what we know about the cannabis plant from research. “We’re really at this point trying to play catch-up.” The complexity of the cannabis plant compared to other medications creates problems for the FDA when deciding how to regulate it.
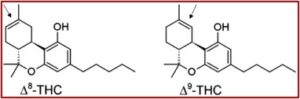
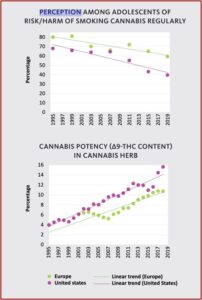
Cannabis contains over 500 distinct compounds and over 100 different cannabinoids. THC, delta-9-tetrahydrocannabinol, is the main psychoactive cannabinoid. CBD, cannabidiol, is a non-psychoactive cannabinoid with demonstrated medically useful properties. Selective breeding of cannabis over the past two decades has increased THC levels, while reducing the CBD levels. “There are concerns that the significantly elevated THC content of modern cannabis may be exacerbating the potential health detriments, particularly in relation to cognitive and psychiatric disorders.”
STAT raised several concerns that should be considered by medical research into—and our understanding of—cannabis. First, will reclassification have much of an impact on clinical trials into marijuana’s potential as a medicine? Many top cannabis researchers are skeptical.
The FDA requires research extensive tests for a new drug in humans to submit an extensive amount of data outlining the drug’s absorption and metabolism rates and toxicology studies on lab animals. Cannabis is no different. This is to help protect participants in clinical trials from adverse effects from potentially dangerous drugs. Researchers have complained the FDA’s review of INDs (investigational new drugs) has been too strict and slow, creating a backlog of studies waiting to begin. More than 150 research applications for studies into cannabis were pending before the FDA as of March 2024, according to a recent to the head of the Drug Enforcement Administration.
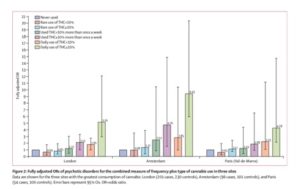
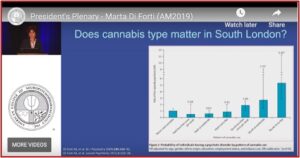
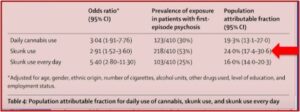
Second, there are many unanswered questions about cannabis from a basic scientific perspective. For example, how do the dozens of cannabinoids influence the brain; what changes when people consume cannabis in different forms; and what does this mean for the potential for misuse? There have been multiple reports that high-potency cannabis increases the risk of psychosis, including this recent longitudinal study by Hines, Heron and Zammit. Also see (“Gambling with Cannabis and Psychosis” and “PREPARING to Legalize Cannabis”).
Third, politics could also get in the way, but it’s unlikely that rescheduling will take place before the November 2024 election. The formal regulatory process takes time, particularly when there is one with one such “historic” implications. STAT said there were over 7,000 comments on the proposed rescheduling by May 30, 2024. There are some Republican lawmakers opposed to the rescheduling, but it remains to be seen if they would sink the proposal in its entirety.
On the other hand, a coalition of Republican and Democratic senators came together on a bill in 2020 meant to lower research barriers and press federal agencies for these answers. It was signed into law in December 2022. Both pro-marijuana and anti-marijuana people have thought further medical research would prove their point. Why don’t we simply wait and find out what the research says?