As I was leaving a rescue mission in Pittsburgh, I saw a homeless man curled up in a fetal position in front of the building. He was unresponsive when I called out to him, so I went back inside and told someone to call 911. While I was doing this, another staff member got Narcan and administered it to the man. When the paramedics arrived, they were eventually able to convince him to go to the emergency department of a local hospital. But he refused further treatment services there and was released.
This is a typical response of those who experience a nonfatal opioid overdose. According to Davis et al in an article published in the Annals of Emergency Medicine, opioid users resist treatment with buprenorphine even though it significantly reduces overdose mortality. In an attempt to minimize this treatment void, some EMS paramedic units are administering buprenorphine to patients almost immediately after reviving them from an opioid overdose. STAT reported back in June of 2019 that New Jersey’s health commissioner authorized paramedics to offer the drug to patients after their overdose has been reversed with naloxone.
The first-in-the-nation model has a twofold purpose, health officials said: Beyond treating the withdrawal symptoms that can result from a naloxone revival, administering buprenorphine on scene could serve as an immediate transition to longer-term treatment.
Dr. Dan Ciccarone, a professor who studies heroin use and the opioid epidemic, said while the prehospital use of buprenorphine comes out of left field, “It’s a potentially brilliant idea.” He sees this as an attempt to treat the person in as well-meaning and patient-centric way as possible. “And that means naloxone plus a softer landing with buprenorphine.” Doctors in numerous emergency departments already prescribe buprenorphine in an effort to provide relief after reversing an overdose. Extending that ability to paramedics “is a new frontier.”
As a safeguard, New Jersey’s 1,900 paramedics will need to obtain permission from the emergency physician overseeing their unit before administering buprenorphine when responding to an overdose call. The supervising physician must have a DEA waiver [and undergo training] to prescribe buprenorphine, a spokeswoman said.
We need to think beyond how we’ve traditionally treated nonfatal opioid overdoses. A CDC press release indicated in the 12-months ending in April 2021, the estimated overdose deaths from opioids increased from 56,064 in April of 2020 to 75,673. Overall drug overdoses increased 28.5% during the same period of time. An interactive web dashboard is available and can gives you predicted overdose data for individual states. The overall increase in overdoses for the United States is 28.5%.
Pennsylvania was among the states hardest hit by the opioid epidemic. In 2018, it had one of the highest death rates from drug over doses, with 65% of 2,866 fatalities involving opioids. Policy responses made to mitigate the spread of COVID-19 in Pennsylvania made the problem worse. Analysis of data from the Pennsylvania Overdose Information Network for both fatal and nonfatal overdoses revealed statistically significant increases across some of the populations most affected by opioids before the pandemic.
In “Assessing the Relationships Between COVID-19 Stay-at-Home Orders and Opioid Overdoses,” the authors said the stay-at-home order in Pennsylvania contributed to a statistically significant increase in opioid overdoses compared with preceding months. See “Unintended Consequences of COVID-19” for more on this topic. It seems this increase in opioid overdoses may have partly motivated Pittsburgh to become only the third city in the country to announce a pilot group of Emergency Medical Services (EMS) paramedics that will administer prehospital buprenorphine.
On November 22, 2021, The Office of Community Health and Safety in Pittsburgh announced paramedics had completed training to administer prehospital buprenorphine and began implementing the practice over the weekend before Thanksgiving. In September, the Pennsylvania Department of Health Bureau of EMS approved the Prehospital Buprenorphine Pilot Program for the City of Pittsburgh’s EMS. The pilot program was designed by the Bureau of EMS in partnership with the Office of Community Health and Safety.
As part of the pilot, Advanced Life Support EMS units will be able to administer buprenorphine to patients experiencing opioid withdrawal regardless if that patient decides to go to the hospital. Patients will then be able to schedule a virtual follow up with the UPMC Medical Toxicology Bridge Clinic to have a consultation with a doctor within 24 hours to get a buprenorphine prescription and be connected to other critical harm reduction resources.
Advanced Life Support EMS units will be able to administer buprenorphine to patients experiencing opioid withdrawal regardless of whether they decide to go to the hospital. Patients will then be able to schedule a virtual follow up to have a consultation with a doctor within 24 hours in order to get a buprenorphine prescription and be connected to other harm reduction resources.
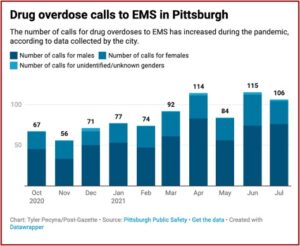
The mayor of Pittsburgh, Bill Peduto, said: “The opioid epidemic has deeply affected so many cities and communities. If tools like buprenorphine exist, we need to have them in our communities and with our emergency medical personnel.” The Pittsburgh Post-Gazette reported there has been a 58% increase in overdose-related calls between October of 2020 and July of 2021—the latest month the city had data on. See the following chart showing the drug overdose calls to EMS in Pittsburgh.
Research shows that buprenorphine-assisted recovery from opioid use decreases the likelihood of recurrent overdoses and death from overdoses while increasing the likelihood of the person engaging in recovery. Dr. Jody Glance said buprenorphine helps patients more comfortably stop using opioids by alleviating their withdrawal symptoms. “Once the person is stabilized on the medication, they will not have the same level of cravings or desire to use illicit opioids.” This stabilization allows the person to engage in activities to support their ongoing recovery.
Dr Glance said some people remain on buprenorphine because they believe it is saving their life. “A lot of people find that the medication is so helpful, that coming off of it is more risky than staying on it.” She added that sometimes people stay on buprenorphine for a long time. Like other chronic, relapsing illnesses, “with opioid use, a lot of times people need a medication on a more long-term basis.” For patients who want hospital treatment, the program allows them to schedule a follow up visit with The UPMC Medical Toxicology Outpatient Clinic to continue taking the drug.
While it is an amazing, almost miraculous tool, bringing relative stability to the lives of opioid addicts, it comes with a price. Buprenorphine is itself an opioid. The DEA classifies it as a Schedule III controlled substance. It’s effectiveness in alleviating withdrawal and minimizing cravings for licit and illicit opioids is based on this pharmacological fact. And long-term use of buprenorphine perpetuates some of the same neurochemical actions found in opioid use disorder.
In her book, Never Enough, Judith Grisel introduced what she said were the three laws of psychopharmacology. They are: 1) all drugs act by changing the rate of what is already going on in the brain; 2) all drugs have side effects; and 3) the brain of someone who misuses drugs adjusts by producing fewer neurotransmitters in the reward circuit, or by reducing the number of receptors that can receive signals. The psychopharmacological action of buprenorphine-assisted recovery on the brain continues to activate these principles.
Not only do we need to bring stability to the lives of addicts after a nonfatal overdose, we need to educate them about the potential consequences they face with long-term use of buprenorphine. Inform them of the cost they’ll pay for a buprenorphine-assisted recovery.
For more information on Judith Grisel and the significance of the three laws of psychopharmacology to addiction recovery, see “Never Enough and No Free Lunch” and “Never Enough and Adaptation.”