Recognizing and Caring for PAWS
I’ve been using Terence Gorski’s material on relapse and recovery for most of my career as an addiction counselor. One of the timeless and helpful topics is his discussion of PAWS—post-acute withdrawal syndrome. He talked about PAWS within Staying Sober, a book he co-authored with Merlene Miller in 1986. There is a briefer discussion of his PAW symptoms in a booklet, The Relapse Recovery Grid embedded in his presentation of the Phases of Relapse. I even found something on Facebook, on April 5, 2012: “Post-Acute Withdrawal Syndrome – What You Need to Know.” Let’s see how Gorski’s description of PAWS holds up after 35 years.
According to Gorski and Miller, PAWS is “a bio-psycho-social syndrome. … It results from the combination of damage to the nervous system caused by alcohol or drugs and the psychosocial stress of coping with life without drugs or alcohol.” They grouped PAW symptoms into six types that continue to appear in other presentations of PAWS, a few of which we will look at later. Their six types of PAW are: an inability to think clearly, problems with memory, emotions that range from overreaction to numbness, sleep-related problems, physical coordination problems and stress sensitivity.
Gorski said difficulty thinking clearly was the most prominent symptom, where addicts who just completed acute withdrawal (detox) regularly have problems with simple problem-solving and decision-making. At this time in recovery, individuals often have difficulty with abstract concepts and problems concentrating. They also have rigid and/or repetitive thinking patterns. Memory problems are particularly frustrating in early recovery, as they are evident when someone is trying to learn new skills and behaviors to support their abstinence.
Stress, the sixth symptom, seems to worsen memory problems. In The Relapse Recovery Grid, Gorski said problems managing stress are two-fold. First, there is brain dysfunction from long-term alcohol or drug poisoning. Second, as the brain becomes overloaded, it shuts down temporarily. The first evidence of this is seen in emotional numbness.
When emotionally numb, recovering people cannot recognize the minor signs of daily stress. When the stress does break through into consciousness, they tend to overreact. Stress sensitivity causes them to amplify, magnify and intensify whatever feelings they are experiencing. When they do recognize stress, they are not able to relax. They get so tense that they are not in control of themselves. Sometimes the stress is so severe they can’t function normally.
Although physically stable enough to be free from the medical supervision of detox, individuals may have continued physical symptoms of withdrawal in sleep difficulties and physical coordination problems. Sleep problems can continue for months, sometimes longer. “The most important thing to understand about PAWS is that each person must work through it in their own time. Nervous system damage typically requires from six to twenty-four months for recovery.”
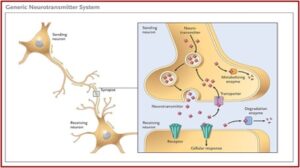
One of the advances over the past 30 some years with addiction research has been the growing understanding of the importance of neurotransmitters to developing and treating alcohol and drug dependence. Neurotransmitters are naturally occurring chemical substances that act like messengers, transmitting a message from one brain cell or neuron across a gap called a synapse to another brain cell. And when you do something to stimulate or alter one neurotransmitter, you usually disturb several others. The neurotransmitters important to addiction are: serotonin, norepinephrine, endorphin, endocannabinoids, (yes one for cannabis or marijuana) GABA, glutamate and dopamine. They are released from the sending neuron and absorbed by the receiving neuron. See the following graphic.
 Naturally occurring opioids or endorphins reduce the amount of GABA released. Reducing GABA increases dopamine. Dopamine is the neurochemical that reinforces the brain’s desire to repeat a certain behavior by signaling we are about to have a pleasurable or meaningful event. It is also involved in energy and attention. When our dopamine levels are low, our energy levels are low.
Naturally occurring opioids or endorphins reduce the amount of GABA released. Reducing GABA increases dopamine. Dopamine is the neurochemical that reinforces the brain’s desire to repeat a certain behavior by signaling we are about to have a pleasurable or meaningful event. It is also involved in energy and attention. When our dopamine levels are low, our energy levels are low.
Norepinephrine is responsible for attention and alertness. Glutamate is the main excitatory neurotransmitter. Serotonin has over 17 kinds of neuronal receptors and can both excite and calm us. Some serotonin receptors, when activated, increase anxiety and alertness, others are more calming. Endocannabinoids are involved in regulating mood, appetite, pain, cognition and emotions. Acetylcholine is another neurochemical that activates nicotinic receptors.
Cocaine, amphetamines and alcohol use reduces the uptake of dopamine (reinforces euphoric activity and tells us to remember it) and increases the amount of glutamate (major excitatory neurotransmitter). In high doses, they also inhibit monoamine oxydase A (MAO-A). In other words: “Large surges of dopamine ‘teach’ the brain to seek drugs at the expense of other, healthier goals and activities.” The person’s body has adjusted to having excessively high amounts of dopamine and glutamate and excessively low MAO-A. Our brain seeks to maintain a neurochemical balance, so it alters its structure as it seeks a balance or a “new normal.” Without the drug (cocaine, amphetamines, alcohol, etc.) anymore, it doesn’t have enough receptors for the glutamate and dopamine, and it has too many receptors for the monoamine oxydase.
Drugs and neurotransmitters activate the same receptors. The following table lists the neuronal receptors involved in drug actions.
| Drug | Neuronal receptor |
| opioids | Endorphins (4 types) |
| cocaine | Dopamine (5 types) |
| Prozac, SSRIs | Serotonin (over 17 types) |
| nicotine | Acetylchloline (8 types) |
| cannabis | Endocannabinoids (2; CB1, CB2) |
| benzodiazepines | GABA? (5 types) |
| alcohol | GABA? (5 types) |
In summary, with chronic substance use, the brain comes to rely on the drug to maintain the high degree of pleasure associated with the artificially elevated levels of neurotransmitters in its reward circuits. The brain then adapts to these high neurotransmitter levels by making new receptors or decreasing the production of neurotransmitters. This leads to depression or anxiety and cravings if drug use stops and neurotransmitter levels return to normal because there are now too many receptors for normal levels of neurotransmitters.
The Hazelden Betty Ford Foundation discussed Post-Acute Withdrawal Syndrome, describing it as the brain recalibrating itself after active addiction. “Think of the withdrawal syndrome as the brain’s way of correcting the chemical imbalances suffered during active addiction.” They suggested that PAWS occurred most commonly and intensely in people with alcohol and opioid addiction, as well as those with an addiction to benzodiazepines. They expanded Gorski’s six symptoms, adding urges and cravings, irritability or hostility, fatigue, anxiety or panic, depression and lack of initiative. Like Gorski, they suggested some coping strategies for getting through PAWS.
YouTube has multiple videos of Terence Gorski and his work on relapse prevention. Just go to YouTube and search for “Terence Gorski.” There are also multiple videos on PAWS. I will only note two, one from Vertava Health, that is about 12 ½ minutes long: “What Is Post-Acute Withdrawal Syndrome (PAWS)?”And one from AllCEUs Counseling Education by Dr. Dawn-Elise Snipes, that is 53 minutes long, “Post-Acute Withdrawal Syndrome (PAWS) in Addiction Recovery.”
In the Vertava video, it said PAWS symptoms often present themselves to people after they detox from drugs and alcohol. The symptoms are often hard to see, as they are more psychological than in acute withdrawal. “This is a pain that can’t be measured. But it can be just as big a risk for relapse.” In PAW, the brain is trying to re-acclimate to a normal state, “where it would have been prior to the drug or alcohol use.” One of the speakers essentially repeated Gorski’s six types in saying there can be an increased stress response, irritability, inability to control emotions, anxiety, depression, difficulty thinking clearly or an inability to focus, difficulty completing tasks that used to be easy to do, memory problems, sleeping problems.
PAWS, when you hear that anacronym, it sounds like something you want to play with. But in all actuality, it’s something that’s gonna play with you. It’s going to get you before you get it, if you are not aware of it. I mean it will come up behind you and attack you. You have no idea it’s coming.
AllCEUs is an online educational organization offering over 900 free videos on mental health and addiction issues on their YouTube channel. Professional counselors can view ALLCEU videos for various continuing education and online certification training needs. Dr. Snipes gives a thorough and understandable talk on PAWS in “Post-Acute Withdrawal (PAWS) in Addiction Recovery.” She said after people get past the acute withdrawal phase, they will have some days where they feel pretty good and some days when they can re-experience symptoms they felt during detox. They need to know this is normal. And they have to have a plan to deal with these symptoms because in the past they used as a result of experiencing them.
PAWS, post-acute withdrawal syndrome, is the result of changes in the brain after you stop using drugs and alcohol. As Judith Grisel put it in Never Enough, “The brain’s response to a drug is always to facilitate the opposite state; therefore, the only way for any regular user to feel normal is to take the drug.” Even prescription medications can produce PAWS. Acute withdrawal occurs up to about two weeks after the person stops using drugs or alcohol; Post-acute withdrawal symptoms begin after acute withdrawal and can occur for up to one, or sometimes two years, after stopping.
Terence Gorski indicated PAW symptoms peak in 3 to 6 months and then declined over time, with stress sometimes triggering a spurt of PAWS. PAWS is influenced by age, gender, the length of time a person was actively using, the amounts of drugs used, physical health and any underlying mental health symptoms. How old a person was when they began using is also important because they may have done some permanent damage to their brain. Their brains may not be able to fully return to pre-using levels of functioning.
Think of PAWS as the brain’s way of correcting the chemical imbalances suffered during active addiction. Your brain needs to slowly reorient itself. There are two possible outcomes here: either resume drug use to get the additional artificial boost to the neurotransmitters, or don’t use and wade through the time and process of the brain healing itself.
Post-Acute Withdrawal symptoms can include:
•emotional outbursts or numbness (lack of emotion)
•anxiety or irritability
•depression or anhedonia (inability to feel pleasure)
•difficulty dealing with stress
•fatigue
•problems sleeping
•memory problems making it hard to learn new things
•trouble thinking clearly, making decisions, or solving problems
•and balance, dizziness and physical coordination problems
The symptoms in bold are the six types of PAW symptoms identified by Terence Gorski over thirty years ago. People may have more depression and anhedonia (the inability to experience pleasure) if their drug of choice was a stimulant like cocaine or meth. If their drug of choice was a depressant (opioids, alcohol, benzodiazepines) they may have more anxiety and irritability. Stress and fatigue occur with low dopamine.
Sleeping problems can include strange dreams or changes in sleeping patterns. serotonin, one of the neurotransmitters that gets out of balance with chronic drug use, breaks down in the body to make melatonin, which helps us drift off and stay asleep. In early recovery you also need to reset your circadian rhythm, a natural, internal process that regulates the sleep-wake cycle. Up-and-down serotonin levels can lead to sleep problems; anxiety can interfere with sleep. It’s important to realize this and be mindful of things people can do to improve their sleep problems, like lower their caffeine intake, exercise, practice mindfulness. Memory problems make it hard to learn new things. When dopamine is low, it influences our concentration is low. When norepinephrine levels are low, our concentration is low. The brain is worried about recovery—rebalancing and repair; it’s not trying to focus on learning new things.
Adenosine is a neurotransmitter to be aware of. As it builds up in our brain, it causes us to be sleepy. Deep sleep at night clears out the adenosine. In early recovery because of PAWS, people don’t get good sleep. When they don’t get good sleep, the adenosine doesn’t get cleared out and contributes to them feeling foggy the next morning. Caffeine binds to adenosine receptors and keeps the adenosine from binding to the receptor and making us feel sleepy; it makes us more alert.
Interventions to help people in early recovery with their PAWS, to help them self-regulate, include meditation and deep, focused breathing, relationships with sober support people, exercise, sleep, restabilizing their circadian rhythm, awareness and mindfulness (self check-ins) pleasurable activities, eating healthfully, relaxation. In early recovery people are fatigued and tired, because of low dopamine, but too much sleep messes up the circadian rhythm and your brain doesn’t know when it’s supposed to sleep. Naps should be limited to between 20 and 45 minutes so they don’t go into a deep sleep state. Encourage people to go to sleep at a regular time. Mindfulness is an important part of preventing relapse. As the person grows in their awareness of the sometimes, subtle changes that occur, they can do something about them. Eating healthfully is important, because most neurotransmitters are made in your gut. Relaxation is both physical and mental. What things do people do for relaxation? Relaxation and GABA go hand in hand.
In summary, according to Dr. Snipes PAWS is an expected issue for at least the first year in abstinence as the brain and body recover. PAW symptoms are the result of the brain’s neurotransmitter system being disrupted by drug and alcohol abuse. In early recovery, it is not helpful or realistic to ignore or minimize PAW. A primary goal in early recovery should be to minimize stress.
There are a multitude of voices today talking about the dangers of PAWS to someone attempting to get clean and sober. While there are more specifics on the effects of PAWS to the neurotransmitter systems in the brain, Gorski’s discussion of how to recognize and care for PAWS still holds up after 35 years.

