Tell It Like It Is
Recently I saw one of the ubiquitous “ask your doctor if … is right for you” commercials for Rexulti. The slick 90-second ad tells you that when Rexulti is added to your antidepressant, it has been shown to reduce symptoms of depression. The smiley faces used by the actors illustrate how: “Even when you’re taking an antidepressant, you may still be struggling with depression.” You learn that 2 out of 3 people taking an antidepressant may experience unresolved symptoms of depression; and that antidepressants can cause unusual changes in behavior, worsening depression and thought of suicide, especially in those 24 and younger. But you never learn that Rexulti is not an antidepressant.
The commercial never claims Rexulti is an antidepressant, but it clearly leads its viewers in that direction. Counter intuitively, in order to make the case for using Rexulti, it not-so-subtly tells you that antidepressants alone aren’t always effective, since 67% of people taking them have “unresolved symptoms” of depression. But then you learn Rexulti has been shown to reduce symptoms of depression when it is added to an antidepressant. The message is that Rexulti is effective relieving symptoms of depression. But let’s deconstruct what the commercial is telling you even further.
In the mix of the marketing rhetoric, you hear a litany of possible adverse medication side effects. The initial side effects are found with antidepressants: there could be unusual changes in behavior, worsening depression, even thoughts of suicide. “Antidepressants can increase these in those 24 and younger.” This information is legitimately about the side effects from antidepressant medications. See “Antidepressant Misuse Disorder” and “Antidepressants: Their Ineffectiveness and Risks” on this website.
Actually, Rexulti is an atypical antipsychotic or neuroleptic; in the same drug class as Abilify, Zyprexa, Seroquel and Risperdal. The other described side effects and warnings in the commercial are commonly found with atypical antipsychotics. See “Adverse Effects of Antipsychotic Medications” by Muench and Hamer for further information.
Looking further, the commercial said: “Elderly dementia patients taking Rexulti have an increased risk of death or stroke.” Antipsychotics were being used to control behavior problems in elderly patients with dementia. Then research demonstrated there was an increased risk of death in the elderly patients given antipsychotics. So the FDA issued a black box warning to that effect. There was also evidence that antidepressants increased the risk of stroke with elderly patients, thus the Rexulti warning. See “Seniors and Antipsychotics” and “Stroke Risk in Elderly Treated with Antipsychotics” for more information on this.
“Uncontrollable muscle movements” in the commercial is likely referring to tardive dyskinesia, a serious and potentially permanent neurological side effect from antipsychotics. The risks for developing metabolic syndrome (high blood pressure, high blood sugar, excess body fat at the waist, and abnormal cholesterol levels) are mentioned as well. Tardive dyskinesia and metabolic syndrome are widely acknowledged as potential adverse effects from antipsychotics, but not antidepressants. Try “Blind Spots with Antipsychotics,” Part 1 and Part 2 for a discussion on metabolic syndrome and other side effects from antipsychotics. Stiff muscles, confusion, and high fever are symptoms of “a possible life threatening condition” known as Neuroleptic Malignant Syndrome (See “Neuroleptic Malignant Syndrome”).
So you wouldn’t know Rexulti was an atypical antipsychotic or neuroleptic drug from listening to the commercial unless you knew the above were typical side effects with that class of drug. And you may not even discover this from reading the required Medication Guide, unless you knew what to look for. The FDA’s highlights of prescribing information for Rexulti, all 38 pages worth, does have a more complete discussion of the warnings and precautions as well as the adverse reactions. And Rexulti is referred to there as an atypical antipsychotic. However, in the shorter, two page medication guide, that is made available to individuals filling a prescription for Rexulti, there is no explicit reference to it being an atypical antipsychotic or neuroleptic.
The Rexulti Medication Guide does describe tardive dyskinesia, “problems with your metabolism” and Neuroleptic Malignant Syndrome as possible side effects, which are all potential side effects from antipsychotic or neuroleptic medications. But the only place in the medication guide that the word “antipsychotics” is used is in the section “What should I tell my healthcare provider before taking Rexulti?” There, the medication guide advised that if you become pregnant while taking Rexulti, you should “talk to your healthcare provider” about registering with the National Pregnancy Registry for Atypical Antipsychotics. The only place in the Rexulti medication guide the word “neuroleptic” in mentioned is when it notes how Neuroleptic Malignant Syndrome is a possible side effect.
This rhetorical sleight-of-hand is also present in the medication guides for three other antipsychotics approved by the FDA as adjunct medications for depression. Aripiprazole (Abilify), Olanzapine (Zyprexa) and Quetiapine (Seroquel) all use the same descriptive technique of avoiding reference to the drugs as antipsychotics or neuroleptics in their medication guides. And several have an extended discussion of information on antidepressants. Again, someone not familiar with the medications might think they are taking an antidepressant rather than an antipsychotic medication.
The rational for this would appear to be because the initial market for antipsychotics, treating schizophrenia, is limited. Atypical antipsychotics are now the largest-selling class of drugs in the U.S. with more than $14.6 billion in annual sales for 2014. They also are the class of psychiatric drugs with the most side effects. See “Wolves in Sheep’s Clothing” and “Abilify in Denial” for more on these observations.
Another piece of information about Rexulti in contrast to the other antipsychotics approved as adjunct medications for depression is that it is the only one still on patent. Rexulti patents don’t expire until February of 2027 Abilify, Zyprexa, and Seroquel have all been approved as generics. So Otsuka Pharmaceutical Company Ltd. has the potential for much greater profits from Resulti over the next ten years than the generic pharmaceutical companies have for the off-patent atypical antipsychotics.
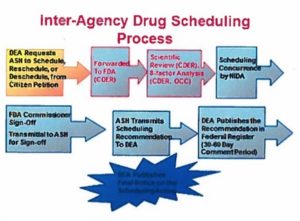
There seems to be a general trend when discussing psychiatric medications to avoid any reference to them as atypical antipsychotics or neuroleptics. You can even see this in the FDA press release for the approval of Rexulti in July of 2015. This means a consumer looking for information on the potential adverse effects from an atypical antipsychotic may have some difficulty finding and then understanding what the risk is for them to take the drug.
For clarity’s sake, I think the FDA should require all consumer medication guides to clearly identify the drug class for approved psychiatric medications. They should also direct a patient to where they can find a more complete discussion of the potential adverse effects of the medication than what is contained within the brief summary of the medication guide. Confusing discussions of depression, its symptoms and the side effects from antidepressants included in antipsychotic medication guides should be clarified or removed entirely by the FDA. Additionally, there should be a truth in advertising requirement that tells it like it is for all psychiatric drug advertisements. An antipsychotic by any other name is still an antipsychotic and the commercials should say so.