The Opioid-Heroin Cycle
Since the death of Philip Seymour Hoffman on February 2, 2014, there has been a series of calls for the distribution of naloxone or Narcan, which is a prescription medication that reverses an opioid overdose. But it seems that the price of Narcan has doubled over the past year. The Fix and others report that the price of naloxone has recently gone from $51.50 per kit, to nearly $100 per kit. These are the Luer-Jet™ kits sold by Amphastar Pharmaceuticals, the only US company currently selling nasal kits. There is a cheaper injectable form of narcan, but it is supposed to be less user friendly.
Within four days of Hoffman’s death, The New York Times published an article by an emergency physician, noting how greater availability of Naloxone could prevent deaths. He referred to a report in the Annals of Internal Medicine that suggested up to 85 percent of users overdose in the presence of others, providing the opportunity for others to intervene. In Forbes Magazine David Kroll said the CDC reported that naloxone was used in over 10,000 opioid-overdose reversals between 1996 and mid-2010. He also expressed his concerns over potential shortages of naloxone.
Victoria Kim for The Fix reported that Amphastar’s president blamed the price increase of their naloxone product on “steadily increasing” manufacturing costs. But Matt Curtis, the policy director for a New York advocacy group said there had been a fairly steady price for several years. “Then these big government programs come in and now all of a sudden we’re seeing a big price spike. . . . The timing is pretty noticeable.” The Hill reported that Senator Bernie Sanders and Representative Elijah Cummings sent a letter to Amphastar complaining about the price increase and how it is “an obstacle in efforts by police departments to equip officers with the drug.”
Areille Pardes of Vice said that after the CDC said there was an opioid epidemic in 2008, the manufacturer of naloxone, Hospira, increased the price of a dose of naloxone from $3 to a little more than $30. Pardes also reported that the supposed difficulty of a lay-friendly delivery system has also been used to justify the high costs of epipens (around $400) and the naloxone auto-injector, EVIZO (Over $600 for a kit of 2 auto-injectors at Walmart, Sams Club, Target and other retail outlets). However a study found few differences between trained and untrained overdose rescuers in their abilities to use the syringes in a naloxone rescue kit. “Anyone with common sense could figure it out, even without training.”
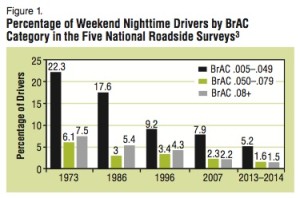
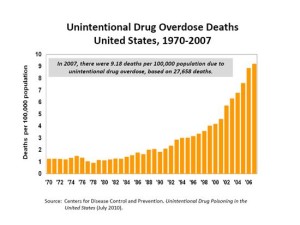
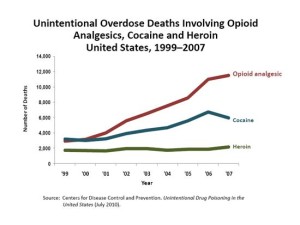
It does seem that the timing of the price increases for naloxone (a generic drug) and its delivery systems occurred just as the epidemic of overdoses took place. The CDC reported in a March 2015 NCHS Data Brief that from 2000 to 2013 the rate of drug overdoses quadrupled, from .7 deaths per 100,000 to 2.7 deaths per 100,000. Overdoses are now the number one cause of injury-related death in the US. While the overdose deaths involving (prescription) opioid analgesics have leveled off in recent years, those from heroin have almost tripled. See Figure 1 of the NCHS Data Brief. While the heroin overdose rates increased among all age brackets, the highest rate of increase was among 25-44 year olds. Geographically, while there were increases in all regions of the country, the greatest increase took place in the Northeast and the Midwest. See figure 5 of the NCHS Data Brief.
There is some sense that effort to curb problems with overprescribing pain medications has inadvertently led to a boom in the misuse of heroin. Richard Juman reported for The Fix that while some treatment providers suggest that is the case, others note that there is evidence that heroin use was increasing before any state or federal interventions with prescribed opioids were implemented. According to Andrew Kolodny, MD:
The idea that efforts to curb prescription drug misuse have led to a spike in heroin use or overdose has become a common media narrative, but the facts don’t support it. It is the overprescribing of opioids itself that has caused increases in opioid addiction of all kinds, not the efforts to control the prescribing. The transition from prescribed opioids to heroin has been happening since the beginning of the epidemic, and there is no evidence that the interventions brought forth to reduce the overprescribing have been fueling the increase in heroin use or overdoses. Because of the epidemic of opioid addiction, you now have markets for heroin that you didn’t have in the past. So there has been an increase in heroin overdose deaths, but that increase was prior to states’ implementation of Prescription Monitoring Programs or any of the changes from the FDA.
I tend to agree with Dr. Kolodny’s assessment. There is a price factor in the shift for many opioid users switching to heroin. And there has been a global market increase in heroin production that paralleled the rise of prescription opioid use. Increased heroin use in the US is market driven. What does seem to be related to increased heroin availability in the US is the diversification of Mexican drug cartels into growing opium poppies, as their market for marijuana dries up. See “The Economics of Heroin.”
There is something very wrong with the cycle of Pharma marketing for increased use of opioids, leading to overprescribing opioids, leading to increased heroin use and increased overdoses, leading to an increased need for narcan, leading back to increased profits with drug companies, where the cycle began. The ouroboros pictured above is a symbol in Greek mythology of a dragon eating its own tail. It symbolizes something that constantly re-creates itself, which seems to be happening here with the opioid-heroin cycle.