High on Flakka
 Flakka continues to make the news and it seems to be spreading beyond its popularity in South Florida. A Fusion article showed that while 48% of the confirmed cases of flakka in the first half of 2014 were from Southern states, 27% were in the North East and 23% in the Midwest. “In 2015, individuals have been arrested for dealing Flakka in Illinois, Iowa, New York, and Minnesota.”
Flakka continues to make the news and it seems to be spreading beyond its popularity in South Florida. A Fusion article showed that while 48% of the confirmed cases of flakka in the first half of 2014 were from Southern states, 27% were in the North East and 23% in the Midwest. “In 2015, individuals have been arrested for dealing Flakka in Illinois, Iowa, New York, and Minnesota.”
But the largest epicenter outside of Florida may be southern Ohio around the town of Ironton. In January of 2015, two brothers, residents of Ironton, were arrested and charged with trafficking in alpha-PVP (flakka). Detective Joe Ross said they were having a lot of complaints from citizens about the sale of Alpha-PVP. “It’s been a big problem here in the city and in the county.”
In Broward County, Florida, flakka accounted for 34% of their crime lab reports. In the ten months prior to August 2015, 33 people died from flakka-related overdoses in Broward County alone. Hospitals in Broward County reported seeing up to 20 flakka-related patients a day. Two men in Broward County pleaded guilty in August 2015 to importing more than 24 pounds of the main ingredient in flakka from China. Also see “Flack from Flakka” and this article by McCarton Ackerman on The Fix.
Flakka is more than just fodder for crazy news stories about naked people running around saying they are Satan, or trying to break into police stations to avoid get away from 20 cars chasing them and trying to kill them. It has also caught the attention of respected addiction professionals—Terence Gorski and researchers at The Scripps Research Institute.
Scientists at The Scripps Research Institute (TSRI) have found that flakka (alpha-PVP) seems to be equivalent to MDPV (bath salts). The study was a classic animal pressing a drug-delivery lever study; and the rats increased their lever pressing for the drug as the 20 daily sessions progressed. “When the researchers increased the number of lever presses required to get one dose, the animals kept pressing—for up to hundreds of presses per dose.” Those rats must have REALLY like their flakka. Head-to-head tests of flakka and bath salts showed an almost identical potency for inducing lever presses. This suggested to the researchers that the horror stories about flakka may have been overblown. An abstract for the 2015 study discussed by Aarde et al., is here.
They noted how a 2013 study, also by Aarde et al., found that bath salts induced far more drug-seeking lever presses among rats than crystal meth. In a TSRI News & Views report of the 2013 study, researchers said the rats worked more than ten times harder to get bath salts instead of crystal meth. “Animals will self-administer MDPV like no drug I have ever seen.” Where rats would emit about 60 presses on average for a dose of meth, they would emit around 600 for bath salts. “Some rats would emit 3,000 lever presses for a single hit of bath salts.”
Another study, Aarde et al. (2015b), found that bath salts could induce rats to forgo other rewarding behaviors. Rats will almost always respond more to food and tasty flavors than drugs. In this study, wheel running, a normally rewarding activity for rats, declined significantly as they self-administered more bath salts. A subset of the rats didn’t gradually increase their intake of bath salts. Rather, they went from occasional sampling to binging on as much as they could get during a session. “That was when they stopped using the wheel—that very day they binged.” An abstract of the Aarde et al. (2015b) binge study is here.
Terence Gorski wrote an informative summary about flakka on his blog: “Flakka: What You Need to Know.” He said it can cause extreme behavioral reactions and there have been reports of long-lasting neurological damage. “It is definitely a dangerous drug that is rapidly entering the drug-using culture.” Citing Jacob Sullim on reason.com, he suggested his readers read his blog to get a balanced view on flakka. Here is a link to Sullum’s article.
Gorski noted how flakka was a relatively new drug, initially available in South Florida in the spring of 2015. It’s a variation of bath salts (MDPV). The active ingredient, alpha-PVP, is a synthetic cathinone, the active ingredient in the khat shrub. Flakka is a stimulant and induces paranoia, psychosis and aggression. In high doses, it leads to “excited delirium,” with high body temperatures rising up to 107F. This leads to many users stripping off their clothes because they feel like they are on fire. When restrained, individuals on flakka scream, flail and struggle to free themselves. The struggling causes high core body temperatures, called hyperthermia, which needs immediate medical treatment to prevent disability and death. The struggling can also cause dehydration.
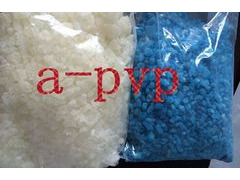
Flakka can be injected, swallowed, smoked or snorted. Especially when smoked or vaped, individuals can overdose on flakka. Remember the overdose deaths in Broward County noted above. It looks like a white or pink crystal; and smells like sweaty socks. Flakka users can become very agitated, making them verbally aggressive and irrational. Muscle tissue begins to break down, releasing proteins and other cellular products into the bloodstream, a condition referred to as rhabomolysis. It can lead to complications such as renal (kidney) failure and in rare cases, death. Gorski also provided this link to the Drudge Report Archives, which tracks news stories on flakka.
If understanding the danger from this drug hasn’t gone from your head to your gut yet, watch a few of these YouTube videos of people on flakka: “Flakka drug effects;” “High on Flakka;” Crazy! Woman High on “Flakka;” “Woman in Florida on Flakka.” Here is a 6 minute video from Fusion: “We spent 24 hours living through Florida’s flakka crisis.”