The Tale of the OxyContin Lie

To tell the tale of OxyContin, we should start with the Sackler family, named by Forbes Magazine as the 16th richest family in the U.S. for 2015 with an estimated net worth of $14 billion dollars. The Sacklers own 100% of Purdue Pharma, which generated more than $3 billion in sales for 2015, most of which came from OxyContin. Separate Sackler-owned companies outside the U.S. with a similar product profile were said to generate as much money in sales to Europe, Canada, Asia and Latin America. In 2007 Purdue Pharma paid $600 million to settle charges it misbranded OxyContin as safer and less addictive than it actually was. Currently, Purdue faces a civil lawsuit in Kentucky with the potential to exceed $1 billion in damages. But I am getting ahead of the story. It all begins with the traditional American success story of an immigrant family who came to America in the early 20th century.
Isaac Sackler immigrated from what is now the Ukraine and Sophie Sackler came from Poland. They ran a grocery in Brooklyn and had three sons: Arthur (1913-1987), Mortimer (1916-2010) and Raymond (1920-2017). All three brothers became psychiatrists. Arthur Sackler was said by the New Yorker to be the “founder” of modern pharmaceutical advertising. His thinking inspired the marketing strategy that would be applied to Oxycontin after his death. The brothers bought a small drug manufacturer in 1952 that would eventually become Purdue Pharma, L.P.
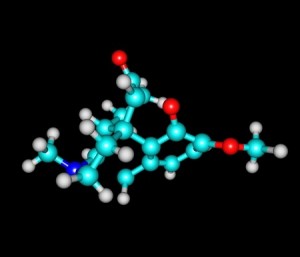
Purdue Pharma initially sold products like laxatives and earwax remover. Then in 1972, the Contin® controlled drug-release system was developed. In 1987, MS Contin®, a controlled release morphine formula was launched. In 1991 Purdue Pharma L.P. was formed, with a focus on pain management. It currently manufactures pain medicines containing hydromorphone, oxycodone, fentanyl, codeine and hydrocodone. In 1993 Purdue established Partners Against Pain® to help alleviate unnecessary suffering of chronic pain care through education. Then in 1996, Purdue launched OxyContin®. In 2010 the reformulated version of OxyContin® was launched. In 2010 the company launched the Butrans® Transdermal system, a buprenorphine-based pain reliever. In 2012 it launched the Intermezzo® sublingual tablet. In 2015 Purdue launched Hysingla® ER, extended release hydrocodone tablets. Also in 2015, Purdue launched TeamAgainstOpioidAbuse.com.
The Contin® controlled drug-release system was marketed as having the potential to minimize or stymie abuse concerns with oxycodone by spreading the drugs effects over 12 hours. Before OxyContin®, oxycodone had only been used for pain relief with cancer patients. “Not long after OxyContin’s launch in 1995, primary-care doctors were prescribing it for an array of painful symptoms.” Mortimer Sackler’s obituary in the New York Times said that by 2001, sales of OxyContin had reached almost $3 billion and accounted for 80% of the Purdue Pharma revenue.
But OxyContin wasn’t as abuse-resistant as it claimed. Reporting for Forbes, Alex Morrell described how the pills could be crushed and the time release mechanism neutralized. Then the drug could be snorted (or dissolved in water and injected) for a heroin-like high. I’ve thought for years that the FDA should have a panel of opioid addicts review every newly proposed abuse-resistant pain medication to brainstorm about possible ways to work around the abuse-resistant technology. The company finally reformulated OxyContin in 2010, which has been speculated by some as contributing to the migration of prescription opioid users to the cheaper and more used heroin.
In 2007 Purdue Pharma, its president, top lawyer and former chief medical officer pleaded guilty to misleading the public about the drug’s risk of addiction. They agreed to pay a total of $635 million in fines. CNBC reported the plea agreement came two days after Purdue agreed to pay $19.5 million to 26 states and the District of Columbia to settle complaints the company had encouraged physicians to overprescribe OxyContin. The state of Kentucky launched an independent lawsuit against Purdue in 2007 alleging false marketing, which is just now coming before a judge. It has the potential for over $1 billion in damages.
Purdue learned from focus groups with physicians in 1995 that doctors were worried about the abuse potential of OxyContin. The company then gave false information to its sales representatives that the drug had less potential for addiction and abuse than other painkillers, the U.S. attorney said.
The LA Times did an investigation of Purdue Pharma and OxyContin and just recently printed their findings. They began by pointing out Purdue Pharma made a bold claim with OxyContin—that it would relieve pain for 12 hours, “more than twice as long as generic medications.” But it seems that for many people, the drug does not last that long and that Purdue knew it. “Even before OxyContin went on the market, clinical trials showed many patients weren’t getting 12 hours of relief.” Since the launch in 1996, Purdue was confronted with additional evidence from a variety of sources, including complaints from doctors, independent research and even reports from its own sales reps.
But Purdue persisted in its claim that OxyContin provided 12-hours of pain relief. It’s high price and huge market was based on this claim. “Without that, it offers little advantage over less expensive painkillers.” When doctors began prescribing OxyContin at shorter intervals than 12 hours, Purdue sent out sales reps to “refocus” doctors on 12-hour dosing. They suggested the doctors prescribe stronger doses, not more frequent ones. But this has the potential to increase the possibility of overdose and death.
Over the last 20 years, more than 7 million Americans have abused OxyContin, according to the federal government’s National Survey on Drug Use and Health. The drug is widely blamed for setting off the nation’s prescription opioid epidemic, which has claimed more than 190,000 lives from overdoses involving OxyContin and other painkillers since 1999.
The LA Times reviewed internal Purdue documents in its investigation spanning three decades, from the conception of OxyContin in the mid-1980s to 2011. The documents painted a clear picture of the development and marketing of OxyContin, how Purdue responded to the complaints about its product, “and their fears about the financial impact of any departure from 12-hour dosing.” Experts said the withdrawal symptoms from OxyContin’s less than 12-hours pain relief, followed by the next 12-hour dose created a cycle of pain and euphoria that fostered addiction. Theodore Cicero, a neuropharmacologist, and researcher into how opioids effect the brain, said this was “the perfect recipe for addiction.”
Now let’s return to the late 1980s. The patent for MS Contin, Purdue’s main source of income, was running out. Executives expected a significant drop in income when the patent ran out. A 1990 memo read: “MS Contin may eventually face such serious generic competition that other controlled-release opioids must be considered.” So they decided to use the Contin technology on oxycodone. Over the next ten years, the company put over $40 million into developing OxyContin.
Multiple clinical trials indicated that OxyContin wasn’t giving 12-hour pain relief. “In study after study, many patients given OxyContin every 12 hours would ask for more medication before their next scheduled dose.” This even happened in the study ultimately used by Purdue to get OxyContin approved as a 12-hour pain relief drug. The official who led the FDA’s review of OxyContin left the agency shortly after the drug’s approval. Within two years, he was working for Purdue in new product development.
Before OxyContin, doctors were hesitant to prescribe narcotic painkillers, seeing them as dangerously addictive. Through organizations like Partners Against Pain doctors were re-educated to “alleviate the unnecessary suffering of chronic pain.” Before the drug’s debut, the minutes of a 1995 meeting indicated a Purdue marketing executive said: “We do not want to niche OxyContin just for cancer pain.” Sales reps urged doctors to try OxyContin with common conditions like backaches and knee pain. “The company invited doctors to dinner seminars and flew them to weekend junkets at resort hotels, where they were encouraged to prescribe OxyContin and promote it to colleagues back home.”
Then came the 2007 lawsuits. Curiously, in all the inquiries into Purdue and OxyContin, the short acting problem was not looked at. Purdue drug reps reported that doctors said the drug didn’t last and many were prescribing it for use three or four times a day. Company officials worried that if OxyContin wasn’t seen as a 12-hour drug, hospitals and insurance companies would resist paying its premium price. So they trained sales reps to convince doctors OxyContin provided 12-hour pain relief. “Purdue held closed-door meetings to retrain its sales force on the importance of 12-hour dosing, according to training documents.”
If a doctor complained that OxyContin didn’t last, Purdue reps were to recommend increasing the strength of the dose rather than the frequency. There is no ceiling on the amount of OxyContin a patient can be prescribed, sales reps were to remind doctors, according to the presentation and other training materials.
There’s more to see in the LA Times article, but you get the sense of the issue. Purdue Pharma responded to the LA Times report, saying it was “long on anecdotes and short on facts.” And it was based on a “long-discredited theory.” They said scientific evidence amassed over more than 20 years supports the FDA’s approval of 12-hour dosing for OxyContin. “The OxyContin label has been updated more than 30 times and at no point did FDA request a change to the dosing frequency.” By the way the medication guide for OxyContin says: “Take your prescribed dose every 12 hours at the same time every day. Do not take more than your prescribed dose in 12 hours. If you miss a dose, take your next dose at your usual time.”
None of the Sackler family has ever been charged in the litigation against Purdue. These days, the family is not involved in the day-to-day running of the company. Throughout their history they have been philanthropic, with donations resulting in the Sackler Library at Oxford University; the Sackler Faculty of Medicine in Tel Aviv, Israel; the Sackler Institute of Biomedical Science at New York University; and the Sackler School of Graduate Biomedical Sciences at Tufts University. But the Sacklers may not be able to be as generous if they lose a major chunk of their $14 billion fortune. A Kentucky judge has ordered the unsealing of secret documents about the marketing of OxyContin in June of 2016, according to STAT. But that’s a tale for another time.