A Regulated Kratom Policy

On August 31, 2016, the DEA announced its intent to temporarily place kratom into Schedule I. This meant that in the DEA’s view, there was no currently accepted medical use for kratom and a high potential for abuse. This led to an immediate and aggressive public backlash. There was a demonstration near the White House, phone calls to Congress, a petition protesting the proposed scheduling with over 100,000 signatures. On October 13, 2016, the DEA announced it would withdraw its intent to temporarily Schedule kratom because of “numerous comments from the public,” but the debate over kratom scheduling was not over just yet.
Natural Products Insider reported that in 2018 the U.S. Department of Health and Human Services, (HHS) officially rescinded the DEA’s request to classify two constituents in kratom, mitragynine and 7-hydroxymitragynine, as controlled substances. But this letter from HHS to DEA was not released to the public until January 2021, when it was made public by The American Kratom Association (AKA). The letter said, “HHS is instead recommending that mitragynine and 7-hydroxymitragynine not be controlled at this time, either temporarily or permanently, until scientific research can sufficiently support such an action.” However, the FDA is still concerned about kratom, as kratom products have been associated with significant safety concerns.
An FDA spokesman said, “While it is important to gather more evidence, data suggest that certain substances in kratom have opioid properties that expose users to the risks of addiction, abuse and dependence.” While the HHS letter did recommend against scheduling kratom, it also stated it was possible that new data and evidence could support scheduling the chemicals in kratom at some future time. “Kratom may have harmful effects, particularly when used with other drugs.” Mitragynine and 7-hydroxymitragynine have many of the properties of an opioid; and enhancing public awareness “that kratom contains molecules that may be potentially dangerous” was encouraged by the HHS.
NPR broadcasted “The Kratom Debate” on its program, Morning Edition. Linda Kline, the owner of Bumble Bee Botanicals, credited kratom with helping her with her mental health. “I went from feeling desperate and hopeless to finding an alternative where I had full control over how I felt.” She couldn’t always find a high-quality supply of kratom, so she began selling kratom herself and now has several stores in California, Idaho and Nevada.
There also was the story of Marco, who struggled with an opioid addiction in high school. He became hooked on painkillers after his dentist pulled his wisdom teeth. Eventually, when he wanted to kick his opioid addiction, he tried kratom and was eventually using multiple kratom capsules daily. During his freshman year at college, he started hyperventilating regularly. The incidents worsened, and led to seizure-like episodes and trips to the emergency room. The doctors were stumped; no one thought to test for kratom.
Marco died in his UC Davis dorm in February 2018, late on a Sunday night. The toxicology report listed “acute mitragynine intoxication” — a chemical constituent of kratom — as the cause of death.
Michael White, of the Department of Pharmacy Practice at the University of Connecticut said, “The data to support either the benefits or the harms for kratom is really, really poor.” He went on to say much of the information available comes from single-case reports. White thought scientists needed to conduct more research before the appropriate level of regulation become clear. He suggested placing it behind the pharmacy counter as with pseudoephedrine.
McLain Haddow, a spokesperson for the American Kratom association thought kratom should only be sold to adults. Haddow added that some manufacturers were adding fentanyl, heroin or morphine to their products to give users a high. “We would like vendors to register their product with the FDA and get a chemical analysis from a certified lab to ensure the only ingredient is the naturally occurring alkaloid in the kratom plant.”
Dr. Scott Steiger, the deputy medical director for an opiate treatment outpatient program said he did not know how to advise patients who wanted to try kratom. “I tell them I just don’t know enough on the basis of science to tell them whether it’s a great idea or not.” He added he’d seen people who use kratom and end up having a very hard time stopping. He doesn’t recommend self-medicating with kratom until more research is available. “We just don’t know enough about this chemical and the long-term use of it to know whether experimenting would lead to complications.”
A Wired article, “Release the Kratom,” said, “They are using the drug for everything from chronic pain relief to replacement for their morning coffee.” People also use it to improve their eye sight, clear up their skin boost their immune systems, or just get high. Some addicts use it to manage or help them get away from their addiction. Faith Day, a kratom business owner in Portland and former addict, said a third of her clientele were looking for a caffeine-free alternative to get through the day: “I’m talking soccer moms.”
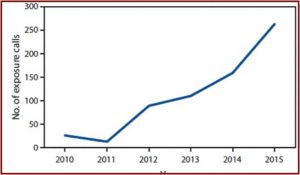
According to Oliver Grundmann, who studies the effects of herbal products on the central nervous system, interest in kratom didn’t become widespread in the US and Europe until the mid 2000s. Grundmann has authored or coauthored several studies of kratom (see here and here), including “Kratom policy, The challenge of balancing therapeutic potential with public safety.” All the article’s authors are engaged in various aspects of kratom research “and it is our intention to provide a fair and balanced overview that can form the basis for informed decision on kratom policy.”
Citing data from the American Kratom Association, the authors said there were more than 1 million kratom users in the US. Given the widespread use of kratom and the extensive media attention it is receiving, the authors said policy makers need to be knowledgeable about the science of kratom. In their article, they sought to answers questions such as: should kratom be classified as an opioid; was it safe; is it effective for pain and OUD management; how serous are the abuse and addiction potentials?
Because of its ability to interact with opioid receptors, mitragynine is often referred to as an “opioid.” Yet it produces physiological, biochemical and behavioral effects that differ from classical opioids. “In light of this evidence, mitraginine and its analogs can best be described as ‘atypical opioids.’”
The authors reported that when used in its traditional context, pure kratom was unlikely to produce serious adverse effects in most users. “In fact, there have been no reported deaths attributed to kratom in Southeast Asia when used in the traditional setting as unadulterated, pure kratom leaf.” At low to moderate doses of 5 g of raw kratom leaves or less, the adverse effects generally seem mild, but can vary between persons. More troubling and serious toxicities are often associated with high dose usage or using concentrated extracts.
The lack of regulation and standardization related to the production and sale of “kratom” products are compounded by unscrupulous vendors selling kratom products adulterated with potentially toxic drugs. “Probably the most notorious example of such adulteration involved a product known as ‘Krypton’, which was touted as a very potent form of kratom.” Sold mainly in Europe, it was a factor in at least nine deaths. Detailed forensic analysis revealed that Krypton was adulterated with the synthetic opioid, O-desmethyltramadol. See “Krypton Can Kill You.”
The unregulated sale of kratom via the internet and deceitful marketing practices may have prompted some individuals to use kratom as a recreational drug. This poorly regulated market, wide distribution, and reported risks of toxicity associated with kratom use, are all likely to have encouraged regulatory agencies to suggest the removal of this product from the market.
While kratom has not been evaluated in the typical controlled clinical trials required by the FDA, many individuals believe it to be a safe and effective alternative to prescription or illicit opioids. “Nonetheless, kratom has a long history of such use that is widely accepted in the general population in Southeast Asia, where it is commonly used as an affordable substitute for street heroin or other opioids.” More than 23,000 comments to the DEA and FDA indicate many Americans have used kratom to relieve withdrawal symptoms and eliminate addictions to licit and illicit opioids.
Thus, even though we do not make the claim that kratom should be viewed as a medically proven effective and safe therapy for OUD, we believe it is warranted to take seriously the extensive user reports and analytical surveillance indicating many people are self-managing their OUD using kratom.
Regular use of kratom, especially at higher doses, can lead to tolerance and dependence. But it seems that abstinence from kratom is typically associated with milder symptomatology than abstinence from classical opioids. Even at high doses, kratom does not seem to severely depress respiration as do classic opioids. “Thus, even though kratom has some potential for abuse and dependence, several investigators have concluded that kratom has both less abuse liability and much lower risk of fatal overdose than traditional opioids.” The study authors said the potential benefits may outweigh the risks.
Kratom is widely used in the West and Southeast Asia as a relatively safe herbal supplement (traditional medicine) for the self-treatment of medical disorders, including pain and OUD. Extensive reports from kratom users, considered alongside limited basic science and clinical research studies, suggest that kratom and its constituent compounds (especially mitragynine) may in fact have beneficial pharmacological and therapeutic properties. Unfortunately, no well-controlled clinical trials have been performed to date to determine the true risks and benefits of kratom use in humans. The high monetary costs of such clinical trials greatly complicate this issue, given that sufficient intellectual property protection to justify the large capital investments necessary for formal drug approval is often challenging to obtain for natural products like kratom.
The conclusions of the authors from their analyses are: (a) kratom and its main constituent alkaloid, mitragynine may be useful for alleviating pain and managing symptoms of opioid withdrawal; (b) while kratom lacks many of the toxicities of classical opioids, there are legitimate concerns about the safety and lack of quality control over “kratom” products being sold in the US; and (c) the issues regarding the safety and efficacy of kratom and mitragynine can only be resolved by further research.
The poorly regulated market, the growing use and reported risks with kratom call for greater oversight or regulation. The suggestions noted above by McLain Haddow of the American Kratom Association are a good start. Both sides of the kratom debate agree that more scientific research is needed and the publication of “Kratom policy” described and linked above is a good start in that direction. Listing kratom as a Schedule I substance at this time will limit the ability to do quality research into the benefits and risks with kratom as it has with marijuana. The abuse and dependence liability with kratom and so-called “kratom” products is real and needs to be investigated with open eyes and not simply minimized.
It’s time for a regulated kratom policy. Let’s not repeat the mistake we made with marijuana by scheduling it before the scientific research supporting its listing can be done.