Coming Up Short with Adderall and Other ADHD Drugs
Since the FDA first announced a national shortage of Adderall in October of 2022, the shortage has now spread to other ADHD medications such as Focalin, Ritalin, Vyvanse, and others. There are an estimated 10 million adults and 6 million children diagnosed in the U.S. with ADHD who are struggling to fill their prescriptions. Medscape said this is especially challenging for people living in rural and underserved areas. The drug shortage is now into its second year, with no apparent end in sight, begging the question how did we get here?
Medscape noted that manufacturers and federal agencies have blamed the rising demand and shortages on each other. Clinicians added that insurers contribute to the shortages by requiring patients to try one, two or three medications before they authorize a more expensive or newer drug like Vyvanse. Congress has also pressured the DEA and the FDA to explain the continuing ADHD medication shortages.
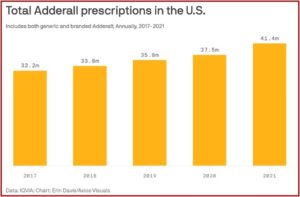
In August of 2023 the DEA and the FDA publicly blamed the manufacturers for the shortages, claiming they were not using up their quotas for the production of controlled substances. Citing CDC data, the agencies claimed when virtual prescribing was widely permitted in 2020-2021 because of the COVID pandemic, prescriptions increased by 10%. Tele-health startups took advantage of an emergency provision during the pandemic that allowed healthcare providers to prescribe controlled substances like ADHD medications via tele-health. They also took advantage of a treatment loophole in diagnosing adult ADHD.
Although there are guidelines for diagnosing and treating children with ADHD, there are no guidelines for adult ADHD in the US. This meant adults can self-diagnose themselves with ADHD after watching some TikTok videos, describe the largely subjective symptoms to their doctor, and get a prescribed stimulant, which they could then use as a study aide or for cognitive enhancement. See “Is Adult ADHD the Latest Fad Diagnosis?”
The failure of manufacturers to increase their production of ADHD medications to meet the increased demand is puzzling. The DEA estimated that drug makers only sold about 70% of their allotted quotas in 2022, “leaving almost 1 billion tablets un-made and un-sold” in the midst of the ADHD shortage. The DEA and FDA agencies said they called on manufacturers to confirm they are working to increase production to meet their allotted quota amount. If they did not want to increase their production, they would be asked to give up their remaining 2023 quota allotment “so it could be redistributed to a drug maker that would increase production.”
According to the American Society of Health-System Pharmacists, some manufacturers have inexplicably discontinued making immediate and/or extended-release ADHD pills, while others gave no reason for their shortage or refused to comment. This has led some impatient adults to turn to online black markets, searching there for “study help” or “study aids.” The Guardian noted where search terms such as “NFL” or “footballs” are also effective, since a 30mg Adderall tablet vaguely resembles a regulation American football.
But legitimacy on the black market is a huge problem. Since the medication shortage began, underground pills sold as Adderall have been found to contain illicit methamphetamine. DrugsData.org found that so-called Adderall pills have been found in circulation from Boston, to San Francisco and LA. In September of 2022 the DEA’s New England office seized 660,000 Adderall pills laced with methamphetamine. The LA Times reported on an elaborate counterfeiting operation in Mexico that “repackages meth as Adderall, Vyvanse and other name-brand ADHD medications.” See “Bad Things Could Happen with ADHD and the Adderall Shortage.”
What may have begun as a little help cramming for a test or temporary help with the demands of a challenging job, can lead to habitual use and a reluctance to forego the perceived “edge” from the medication. Adderall and most other ADHD medications are stimulant drugs with the potential for misuse or addiction. They are listed as Schedule II Controlled Substances, with the same addictive potential as many opioids. A 2018 study by Compton et al in the American Journal of Psychiatry found that among US adults, 6.6% used prescription stimulants; 4.5% without misuse and 1.9% misused them. That is, 28.8% of all those prescribed stimulants misused them. Fortunately, only a fraction of the adult population (.2%) met the criteria for a substance use disorder.
Approximately 16.0 million U.S. adults used prescription stimulants in the preceding year (annual average), 5.0 million misused prescription stimulants, and 0.4 million had use disorders. Cognitive enhancement was the most commonly reported reason for misusing prescription stimulants. Patients who are using their medication for cognitive enhancement or diverting their medication to others present a high risk.
Additionally, a study published in JAMA Psychiatry found a small, but statistically significant association between long-term use of ADHD medication and cardiovascular disease (CVD), particularly hypertension and arterial disease. “In this case-control study of 278,027 individuals in Sweden aged 6 to 64 years who had an incident ADHD diagnosis or ADHD medication dispensation, longer cumulative duration of ADHD medication use was associated with an increased risk of CVD, particularly hypertension and arterial disease, compared with nonuse.” The authors concluded that given that long-term exposure to ADHD medications was associated with an increased risk of CVD, “the potential risks and benefits of long-term ADHD medication use should be carefully weighed.” It was suggested for clinicians to monitor cardiovascular signs and symptoms throughout the course of treatment.
The co-authors of an editorial in the same issue of JAMA Psychiatry said concerns about cardiovascular risk associated with ADHD medications are among the most serious issues to consider when discussing the option of starting medication for ADHD. Medscape reported the increased likelihood of hypertension with long-term use of ADHD medications “cannot be disregarded.” Across the 14-year follow up period, each additional year of ADHD medication use was associated with an average 4% increased risk of CVD, “with a larger 8% increased risk in the first 3 years of cumulative use.” The co-authors said this factor should be carefully weighed against the benefits on a case-by-case basis. Given the observational nature of the study, they could not prove causality.
Hartman et al gave an overview of the comorbidity of ADHD in adults with anxiety disorders (AD), major depressive disorder (MDD), bipolar disorder (BP) and substance use disorders (SUDs) in Neuroscience and Biobehavioral Reviews. Their review found that the prevalence rates of ADs, MDD, BD and SUDs in adults were substantially higher when compared to adults without ADHD. These associations were not modified by sex. The authors proposed monitoring sub-threshold symptoms of these disorders in persons with ADHS to facilitate early detection and preventative measures in order to prevent or postpone the full onset of comorbidity. They suggested further research was needed on whether “adequate ADHD treatment can directly decrease the risk of comorbid disorders.”
These concerns and the supply shortage don’t seem to have affected the income generated by ADHD medication very much. PsychCentral reported that three medications for the treatment of ADHD were among the most profitable for their manufacturers in 2020: Concerta (menthyphenidate, $3.28 billion), Vyvanse (lisdexamfetamine, $3.01 billion), and Adderall, (amphetamine/dextroamphetamine, $2.35 billion). Based on the total number of prescriptions purchased, Adderall was 4th and Concerta was 10th. Vyvanse did not make the top 25 prescriptions listed, likely because its patent did not expire until August 24, 2023.
Yet, not all psychiatrists agree with the DSM-5’s assessment of what constitutes ADHD, let alone its treatment. Sami Timimi said in his article for the International Journal of Qualitative Studies that it required little intellectual effort to conclude the concept and definition of ADHD is full of problems around reliability and validity. “Deciding where to draw the line between what we consider part of the ‘ordinary’ spectrum of behaviours and what we decide is ‘pathological’ is more dependent on cultural than scientific processes.” He said ADHD was not a medical diagnosis, but a cultural construct that spurred the use of stimulant medication, despite the lack of evidence for improved long-term outcomes.
In Saving Normal, Allen Frances, the chairman of the DSM-IV Task Force and part of the leadership for DSM-III and DSM-III-R warned the DSM-5 will mislabel everyday problems as mental illness and turn normal people into “mental patients.” He said, “The easy path to adult ADHD suggested by DSM-5 will mislabel many normal people who are dissatisfied with their ability to concentrate and get their work done, especially when they feel bored and don’t like the work they’re doing.” Symptoms are mostly subjective and based on self-perceptions of poor concentration and task accomplishment. He thought fake adult ADHD would be particularly common in college students, people with demanding jobs, and those who have to struggle to stay awake, like long haul truckers.
Stimulants are among the most effective and safe of medications in psychiatry when given under appropriate supervision for someone who is accurately diagnosed. But they can cause serious side effects in anyone and are especially harmful when taken by someone with another diagnosis that has been misidentified as ADHD (especially substance use or bipolar disorder). The increasing use of stimulants as performance enhancers or for recreation also creates a large and illegal secondary street market.
Frances thought the criteria for a first-time diagnosis of ADHD in adults should be more, not less rigorous. All the many causes of inattention should be first ruled out, and the existing ones be “a continuation of ADHD symptoms that started in early childhood.” He thought any late onset of inattention was caused by something else, not ADHD. “Let’s keep DSM as a manual of mental disorders and not turn it into a vehicle for performance enhancement.”
So, perhaps the shortage with Adderall and other ADHD medications is not such a bad thing. Except, that is, for the people buying what they think is Adderall on the black market. For more information on Adderall, see “Dispatches from the Adderall Epidemic” and its series of articles like: The History of Adderall, My Party Drug of Choice, and Fake Addies.