Overdosing

Melanie (not her real name) was one of the first persons I counseled at White Deer Run in the late 1980s. She was 18 at the time, and a heroin addict before it was being called a national epidemic. She completed treatment; relapsed and returned about a year later as an adult patient. I think she even completed treatment that time as well. I can’t tell you much more about her, except that she was from Philly; and she is the first person I worked with who became an overdose statistic. There have been many more since then.
Most of the places I’ve worked as a drug and alcohol counselor have been within Pennsylvania. So when I heard of the study done by Balmert et al. on the accidental poisoning deaths in Pennsylvania from 1979 to 2014, I was interested in reading it. There aren’t too many ways that statistics, especially death statistics, can be interesting reading. But buried within those tables and figures are people I knew.
Within a data set attached to the study, I found the reported deaths by accidental drug poisoning for the years 1987 through 1989. In 1987, there were 41 individuals between the ages of 15 and 24 who died from accidental poisoning, 6 of whom were female; in 1988 there were 39, 12 of whom were female; in 1989 there were 54, 9 of whom were female. Somewhere in those statistics is Melanie’s overdose.
When I compared those deaths with the last three in the data set, 2012, 2013 and 2014, the stats grew exponentially. In 2012, there were 224 individuals between the ages of 15 and 24 who died from accidental poisoning, 63 of whom were female; in 2013 there were 203, 47 of whom were female; in 2014 there were 277; 70 of whom were female. That’s a lot of Melanie’s.
The CDC published a data brief indicating drug poisoning became the leading cause of injury-related death in 2008, surpassing deaths from motor vehicle accidents. 90% of those deaths were from drug poisoning. From 1999 to 2008 the number of drug poisoning deaths from opioid analgesics more than tripled. “Of the 36,500 drug poisoning deaths in 2008, more than 40% (14,800) involved opioid analgesics.”
Most of those 14,800 deaths involved natural and semi-synthetic opioid analgesics such as morphine, hydrocodone and oxycodone. The number of drug poisoning deaths from methadone, a synthetic opioid, increased sevenfold from 1999 to 2007. Then it decreased between 2007 and 2008. The age group with the highest death rate from opioid poisonings was between 45 and 54 years of age.
In 2007-2008 48% of Americans reported the use of at least one prescription drug in the past month. Not surprisingly, this was related to increases in drug use, misuse and nonfatal health outcomes. Over 5 million reported using prescription pain relievers nonmedically in the previous month.
In 2012 the CDC looked specifically at drug-poisoning deaths from opioid analgesics and heroin. Their report in Health E-Stats noted that from 1999 to 2012 the drug poisoning deaths from opioid analgesics increased from 1.4 per 100,000 in 1999 to 5.1 in 2012. The death rates from heroin overdoses nearly tripled from .7 per 100,000 in 1999 to 1.9 in 2012. The states with death rates significantly higher than the overall U.S. rate of 13.1 per 100,000 included Pennsylvania, Ohio and West Virginia, which had the highest overall rate at 32.0 per 100,000. See the linked CDC reports for more detailed information.
Returning to the Balmert et al. study on accidental poisoning deaths in Pennsylvania, we can see how the Pennsylvania rates compare to those just reviewed. Table 1 in Balmert et al. indicated the overall death rate for Pennsylvania in 2014 was 29.16 per 100,000. The death rate was highest for the 25-34 age group (39.87), and lowest among the 15-24 age group (16.25). See Table 1 in the Balmert et al. article.
Examining the mortality patterns by county showed that the highest rates for males from 2010 to 2014 were in the counties of southwestern PA (the Pittsburgh metro area), the counties surrounding Philadelphia and those near Scranton in the Northeast part of the state. The highest rates for females were in the same areas.
The county level findings provide possible avenues for targeting interventions to areas with the highest mortality from accidental poisoning. Counties with the highest 2010–2014 rates in females are primarily in suburban southwest PA. In males, the highest prevalence rates are more widespread and include both southwest and southeast PA, plus the northeast area including Carbon and Susquehanna. These patterns emphasize that, currently, accidental poisoning deaths especially among white females are occurring in suburban and rural areas. Other area-specific analyses should focus on non-urban mortality patterns.
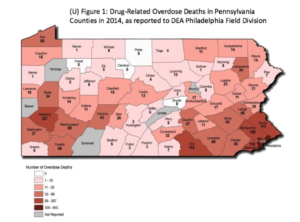
In September of 2014 legislation went into effect allowing first responders to carry naloxone for reversing the effects of an overdose. As of September 1, 2015, 302 overdoses had been reversed with naloxone. The following graphic represents the drug-related overdose deaths by county in Pennsylvania for 2014. See the original here.
In September of 2015, Tom Wolf, the governor of Pennsylvania, announced that the CDC had granted the Pennsylvania Department of Health $900,000 to prevent overdose deaths related to prescription opioids. Governor Wolf said: “Too many citizens of our commonwealth are dying from drug overdose, and Pennsylvania families in hardworking communities are impacted by prescription drug addiction every day.” The “Prevention for States” grant will support 16 states with annual awards between $750,000 and $1 million over the next four years. The goal is to hopefully turn the tide on the prescription drug overdose epidemic by implementing prevention strategies and improving safe prescribing practices.
On March 18, 2016, the CDC published revised guidelines for primary care physicians when prescribing pain medication. Nearly half of all opioid prescriptions are dispensed by primary care clinicians. An estimated 20% of patients with noncancer pain symptoms or pain-related diagnoses receive an opioid prescription. While evidence supports the short-term efficacy of opioids for reducing pain, few studies have assessed the long-term benefits of opioids for chronic pain. An estimated 9.6 to 11.5 million adults (3% to 4% of the adult U.S. population) were prescribed long-term opioid therapy in 2005.
This guideline is intended to improve communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder, overdose, and death.
The guidelines are not mandatory, but if they are followed, maybe the opioid-related overdose deaths will start to decrease and people like Melanie will live instead of die.