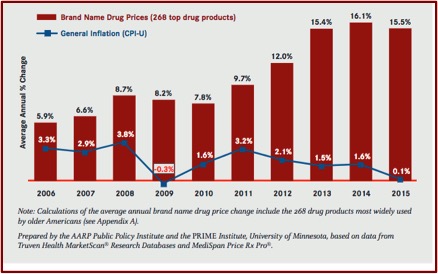
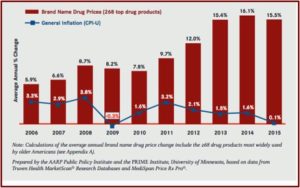
The AARP, the American Association for Retired Persons, completed a report looking at the trends in the retail prices of prescription drugs used by older Americans between 2006 and 2015. And the report’s findings were disturbing. Between 2014 and 2015, the retail prices of 268 widely used brand name prescription drugs increased by 15.5%, the fourth year in a row of double-digit increases. The increase was almost 130 times faster than that of inflation—15.5% to .1% for inflation. The average annual retail cost for one brand name drug was over $5,800 in 2015, almost $1,000 more than the annual cost in 2014. “For the average older American taking 4.5 prescription drugs per month, the annual cost of [drug] therapy would have been more than $26,000 for 2015—more than three times the cost seen 10 years earlier.
This was an industry-wide trend, as the prices of the identified drugs, from all 35 drug manufacturers with at least two brand name drugs assessed within the study, increased faster than the rate of general inflation in 2015. “All but one of the therapeutic categories of brand name drugs had average annual price increases over 5% in 2015. . . . The higher costs are typically passed on to the consumer in the form of higher cost sharing, deductibles, and premiums.” These increases were far beyond the price increases for other consumer goods and services between 2006 and 2015. The following graph compares the annual price of brand name prescription drugs to rate of general inflation for the corresponding year.
The next figure illustrates how the average annual cost for widely used brand name drugs by older adults grew more than 300% from 2006 to 2015. The Medicare Part D program was first implemented in 2006. Older Americans fill an average of 4.5 prescriptions for medications per month. If they used brand name prescription drugs, their average annual retail cost for medications would be $26,132. “This annual retail cost of brand name prescription drugs exceeds the median annual income for a Medicare beneficiary ($24,150).”
 It is no coincidence that these price increases for medications commonly used by older adults occurred after The “Medicare Prescription Drug, Improvement, and Modernization Act” was approved in 2003. “It expressly prohibited Medicare from negotiating bulk prescription drug prices.” But the Veterans Health Administration and the Defense Department were allowed to negotiate lower prescription drug prices. Prohibiting Medicare from negotiating bulk drug discounts seems directly related to increases in medications noted above.
It is no coincidence that these price increases for medications commonly used by older adults occurred after The “Medicare Prescription Drug, Improvement, and Modernization Act” was approved in 2003. “It expressly prohibited Medicare from negotiating bulk prescription drug prices.” But the Veterans Health Administration and the Defense Department were allowed to negotiate lower prescription drug prices. Prohibiting Medicare from negotiating bulk drug discounts seems directly related to increases in medications noted above.
The AARP Public Policy Institute found there were six specific brand name drugs with the highest percentage changes in retail price from 2006 to 2015. FIVE of them were from the same pharmaceutical company—Valeant. One mg and two mg tablets of Ativan (for anxiety) increased 2,873% and 2,080% respectively in their retail price. Cara .5% cream (certain skin disorders) increased 2,395%. Wellbutrin (for depression) increased 1,185%. Zovirax 5% cream (certain skin disorders) increased 783%. Eli Lilly’s Humulin R (U-500) 500 units/ml, an insulin drug used to treat diabetes, ONLY increased 530%.
If recent trends in brand name drug prices and related price increases continue unabated, the cost of drugs will prompt increasing numbers of older Americans to stop taking necessary medications due to affordability concerns. Continued excessive brand name drug price increases will also lead to increased cost sharing and premiums, which could ultimately make health care coverage unaffordable and lead to poorer health outcomes and to higher health care costs in the future.Given that health care reform expanded the number of people using prescription drugs, it would have been reasonable to expect smaller brand name drug price increases. Instead, brand name drug prices have accelerated substantially. Clearly, the economics of the pharmaceutical market are not working as expected.
Andy Slavitt, when he was the acting administrator for the Centers for Medicare & Medicaid Services, told the pharmaceutical industry in November of 2016 at a conference that increased medication costs were pervasive. Total prescription drug spending in 2015 was $457 billion, 16.7% of health care spending. Mylan’s Epipen was not even in their top twenty list for high price increases for 2015. Specialty drugs (like hepatitis C drugs) were a big part of the cost increase. They accounted for 31.8% of spending, while representing only 1% of prescriptions. Out of the 20 drugs with the highest per-unity cost increases in Medicaid, seven were generic drugs. Those increases were not to recoup drug development expenditures. See “Pharma’s not Getting the Message” for more on this topic.
The NYT reported there has been a sharp rise in polypharmacy, the use of three or more psychotropic drugs, with older adults. Almost half of these patients DID NOT have a diagnosis for mental health or pain disorder on record. Dr. Maust, a geriatric psychiatrist and lead author of the study, told Psychiatric News: “This begs the question of why physicians are exposing patients to all the risks of these medications, but not for the diagnoses they are intended to treat.” He thought the pattern suggested some inappropriate prescribing. Dr. Dilip Jeste, a geriatric neuropsychiatrist and past president of the American Psychiatric Association, said he was stunned to hear “that despite all the talk about how polypharmacy is bad for older people, this rate has doubled.” Over 90 percent of the office visits examined in the study occurred outside the psychiatric setting.
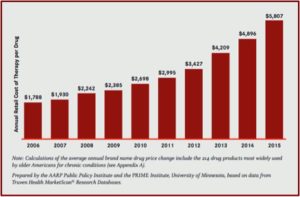
The AARP Public Policy Institute reported that 65% of adults over the age of 65 reported using 3 or more prescription drugs in the past 30 days. Ninety percent reported using one prescription drug in the past 30 days, while 39% said they used five or more. See the following figure from “Prescription Drug Abuse Among Older Adults.”
 Disturbingly, this study looked at polypharmacy with medications noted within the Beers Criteria, named after its originator with the American Geriatrics Society twenty years ago. The Beer Criteria lists dozens of medications and their mutual interactions that are potentially harmful when prescribed to older adults. “Geriatric medical organizations have long warned against overprescribing to older people, who are more susceptible to common side effects of psychotropic drugs, such as dizziness and confusion.” The Psychiatric News article linked above has a chart of the Beer’s list of CNS medications, their potential risks and alternative clinical recommendations. The classes of medications examined in the study include: antipsychotics, benzodiazepines, sedative hypnotics for sleep (like Ambien), antidepressants (tricyclics and SSRIs) and opioids. An article in the Journal of the American Geriatrics Society on the 2015 updated Beers Criteria is available here.
Disturbingly, this study looked at polypharmacy with medications noted within the Beers Criteria, named after its originator with the American Geriatrics Society twenty years ago. The Beer Criteria lists dozens of medications and their mutual interactions that are potentially harmful when prescribed to older adults. “Geriatric medical organizations have long warned against overprescribing to older people, who are more susceptible to common side effects of psychotropic drugs, such as dizziness and confusion.” The Psychiatric News article linked above has a chart of the Beer’s list of CNS medications, their potential risks and alternative clinical recommendations. The classes of medications examined in the study include: antipsychotics, benzodiazepines, sedative hypnotics for sleep (like Ambien), antidepressants (tricyclics and SSRIs) and opioids. An article in the Journal of the American Geriatrics Society on the 2015 updated Beers Criteria is available here.
Data reported by the AARP Public Policy Institute in “Prescription Drug Abuse Among Older Adults” also noted that older adults has several unique risk factors making them particularly susceptible to misuse of prescription drugs. Misuse is defined here as “the use of prescription drugs in a way a doctor did not direct.” First, older adults use more prescription drugs than any other age group. They also have higher rates of pain, anxiety, and sleep disorders. There could be memory problems that interfere with taking medications at the right time and in the right doses. The high rates of polypharmacy can also lead to potentially dangerous drug interactions.
Age-related physiological changes can also increase the potential for prescription drug abuse. Changes in metabolism, weight, and body fat can affect how a medication works in the body, increasing the potential for misuse and abuse and potentially dangerous side effects. The combination of alcohol and medications can bring about particularly adverse reactions among older adults, as their bodies detoxify and eliminate medications and alcohol more slowly.
Recommendations to prevent drug misuse with older adults include: regular reevaluation of drug dosages to help compensate for physiological changes and declining drug metabolism. Monitor for any inappropriate prescribing of prescription medications. Use of the Beer Criteria discussed above would be helpful. here Because patients often see multiple healthcare providers and obtain multiple prescriptions, keep an eye on a patient’s entire regimen of prescription and nonprescription drug use.
It seems hard to deny that pharmaceutical companies corralled older adults over the past twenty years and branded them as “cash cows” for the drug industry.