Marijuana Policy Has Run Ahead of Science
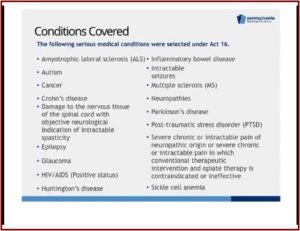
Senate Bill 3 was signed into law by Governor Tom Wolf on April 17, 2016, legalizing medical marijuana in Pennsylvania. The Governor anticipated signing the bill “will improve the quality of life for patients and their families throughout Pennsylvania.” Information on the PA Medical Marijuana Program indicated it would include funding for research to study “the use of medical marijuana to treat serious conditions.” There will also be an advisory committee “that will view these research findings and make recommendations to the legislature for changes to the act.” I’d like to suggest they start with a Harvard-based researcher who is concerned that “policy has outpaced science” when it come to making public health decisions about recreational and medical marijuana.
Staci Gruber is an associate professor of psychiatry at Harvard Medical School and the director of the MIND program (Marijuana Investigations for Neuroscientific Discovery). She has done research on the effects of both recreational and medical marijuana. In an interview with The Harvard Gazette, Dr. Gruber said the science on the health effects of marijuana is not yet settled. “When we think about legalization we always like to have science inform policy. In this particular case, it seems to me that policy has outpaced science.”
She added there is a lot we don’t know about the effects of marijuana. Most of what we do know comes from studies of “chronic, recreational marijuana users.” There are differences between recreational and medical marijuana use, for example with regard to what they use, and how they use. She said there has been well-founded excitement about the potential for medical cannabis use. “[But] there’s a striking paucity of research on the use of medical cannabis.”
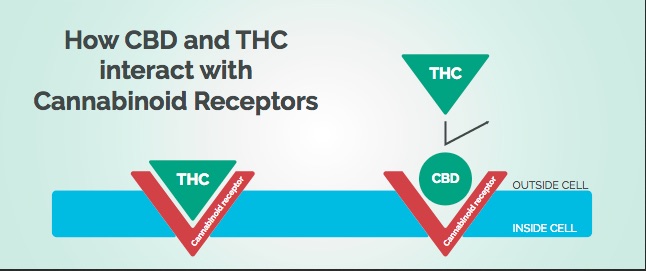
Dr. Gruber and her colleagues discussed the findings in a study of theirs, “Splendor in the Grass?” that looked at the impact of medical marijuana on executive functioning. They acknowledged how the growing body of evidence shows recreational marijuana use adversely effects brain function, especially during adolescence, the critical period of neurodevelopment. But they also theorized the use of medical marijuana (MMJ) may not lead to the same adverse neurocognitive effects. Recreational users, seeking a euphoric, mood altering effect, use products with a high THC content. In contrast MMJ users seek medical relief and use products with a markedly different chemical composition than common recreational products. “These MMJ products are often (but not always) high in other cannabinoids, such as cannabidiol (CBD) which has been touted for its therapeutic potential, and which is not psychoactive.”
The study found that after three months of medical marijuana use, patients (who had previously not been exposed to marijuana) experienced some improvement, rather than the well-documented deficits. “They showed some improvements in measures of executive functions. They also had some improvements in sleep quality and some measures of mood and quality of life.” A subset of people who were using MMJ for chronic pain also reported improvements. Although it was a small sample size, there was a 42% reduction in opiate use. When they analyzed samples of their patient’s products, a number of them were using products high in CBD (cannabidiol) and other non-psychoactive cannabinoids.
Gruber thought there was hope for at least adjunctive therapy, “if not substitution therapy,” for cannabinoids or cannabinoid-based products for individuals currently using opioids. “We’ve seen individuals who’ve stopped using opioids altogether.” That won’t work for everyone. “But that doesn’t mean it’s something that shouldn’t be exploited and explored.”
While future studies are needed to further examine the impact of MMJ, research is impeded by a number of federal and state restrictions. It is imperative, however, that sound research, including well-controlled clinical trials of MMJ products, many of which are already widely used by patients, are thoroughly examined. As the “green rush” pushes forward, gaining momentum as states continue to adopt less restrictive policies, we cannot afford for research to continue to lag behind.
Dr. Gruber said her goal as a scientist was to provide truthful information so all people, regardless of their recreational or medical status, can understand what is in their cannabis or medicine. In pursuit of this goal, Dr. Gruber and her colleague Kelly Sagar continued a discussion of their research with “Marijuana on the Mind?” in Policy Insights from the Behavioral and Brain Sciences. You can also watch an archived webinar by Gruber and Sagar on the same subject, “Marijuana on the Mind: A Primer for Policymakers” on the website Social Science Space, where there are also written answers to some of the questions from the webinar. The presentation exists as an independent YouTube video as well. The audio cuts out a few times, but returns if you continue with the video.
In “Marijuana on the Mind?” Gruber and Sagar gave a helpful review of the history of medical use of marijuana, noting how it was included in the U.S. pharmacopeia (a list of medicinal drugs with their effects and directions for their use) until 1942. They also documented several areas of concern with marijuana, including its adverse effects on cognition, especially executive function and memory; brain development among adolescents; and safety concerns related to the frequency and magnitude of marijuana use as well as its potency.
Marijuana (MJ) use negatively effects executive brain functions (EF) such as attention, decision making, risk taking, inhibition and verbal fluency. An earlier age of onset in using MJ appears to be related to greater impairment on EF. “Several investigations have also noted that lower EF appears to predict increased MJ use.” Several aspects of memory are negatively effects by MJ use. Some evidence suggests increased use and higher exposure to MJ are related to slower psychomotor/processing speed.
The formation of grey matter and whiter matter in the brain is adversely effected by MJ use. Grey matter is responsible for information processing and decision-making. White matter has a critical role in promoting efficient communication within and between regions of the brain. Adolescent MJ users are particularly vulnerable to grey matter reductions; minimal further damage seems to occur after early adulthood. Lower white matter integrity is related to higher impulsivity scores, particularly with early onset MJ users.
MJ users with early onset (prior to age 16) reportedly use MJ nearly twice as often and more than 2.5 times as much relative to late-onset users. Overall, frequency and duration of use appear to be key factors in determining the extent of MJ-related impairment.
Safety concerns with MJ use are on the rise due to the increased potency of marijuana and the use of MJ concentrates. The potency of marijuana has risen nearly 200% since 1995. The use of concentrated MJ products, such as dabs, shatter, wax, budder and others can exceed 60% THC. “Furthermore, these products may also contain residual amounts of solvents (i.e., butane, hexane), often used to make concentrates, which are potentially toxic.” There has been very little research done on cognitive performance or measures of brain structure and function in humans with MJ concentrates. “This raises concern that adverse consequences associated with MJ use may be worse now than in the past, particularly among young users.”
Based upon their discussion, policy recommendation given by Gruber and Sagar include:
- age restrictions based upon evidence highlighting the developmental trajectory of the adolescent brain;
- restrictions on targeting youths in advertisements;
- safe packaging guidelines to prevent the accidental ingestion of edible MJ products by children;
- place limits on THC potency as well as minimums for potentially beneficial cannabinoids in marijuana, like CBD;
- more research on the impact of medical marijuana, which will likely require a lessening of marijuana as a Schedule I substance
As the dialogue regarding legalization of recreational and MMJ continues, perceived risk of MJ use has fallen to an all-time low. Consequently, those with the highest neurodevelopmental vulnerability are using MJ more frequently than in previous years, posing a serious public health issue. A growing body of evidence indicates that relative to non-MJ users, heavy MJ users exhibit poorer performance on cognitive tasks, altered patterns of brain activity, and lower frontal WM coherence, which are highly moderated by age of onset of MJ use. Given the potential therapeutic benefits of MJ, however, it is important to weigh these risks with the benefits. Policy has outpaced science, and eased restrictions allowing citizens to use MJ, in some cases without the benefit of appropriate research. Additional investigation is warranted and necessary to guide informed policy decisions. As states consider legislation for MJ use, it is imperative to determine safe guidelines regarding the impact of MJ on the brain, particularly during critical periods of neurodevelopment.
Dr. Gruber’s research through the MIND program will be extremely helpful for the PA Medical Marijuana Program and state policy makers, such as members of the advisory committee, in making informed public policy decisions with the ongoing availability of medical marijuana in Pennsylvania. The review by Gruber and Sagar of the research relevant the influence of marijuana on cognition, brain structure and brain function in “Marijuana on the Mind?” can be helpful in making future public policy decisions with regard to medical marijuana in the state.
An article cited by Gruber and Sagar, “Cannabis for Medical Use,” should also be reviewed by policy makers, as it is a systematic review and meta-analysis of the benefits and adverse events of cannabinoids. The full text of the systematic review is available. What follows is from the article’s Discussion.
Most studies suggested that cannabinoids were associated with improvements in symptoms, but these associations did not reach statistical significance in all studies. Based on the GRADE approach, there was moderate-quality evidence to suggest that cannabinoids may be beneficial for the treatment of chronic neuropathic or cancer pain (smoked THC and nabiximols) and spasticity due to MS (nabiximols, nabilone, THC/CBD capsules, and dronabinol). There was low-quality evidence suggesting that cannabinoids were associated with improvements in nausea and vomiting due to chemotherapy (dronabinol and nabiximols), weight gain in HIV (dronabinol), sleep disorders (nabilone, nabiximols), and Tourette syndrome (THC capsules); and very low-quality evidence for an improvement in anxiety as assessed by a public speaking test (cannabidiol). There was low-quality evidence for no effect on psychosis (cannabidiol) and very low-level evidence for no effect on depression (nabiximols). There was an increased risk of short-term AEs with cannabinoid use, including serious AEs. Common AEs included asthenia, balance problems, confusion, dizziness, disorientation, diarrhea, euphoria, drowsiness, dry mouth, fatigue, hallucination, nausea, somnolence, and vomiting. There was no clear evidence for a difference in association (either beneficial or harmful) based on type of cannabinoids or mode of administration. Only 2 studies evaluated cannabis.There was no evidence that the effects of cannabis differed from other cannabinoids.
The authors noted there was moderate-quality evidence to support the use of cannabis to treat chronic pain and spasticity. However, the existing evidence suggesting improvements in nausea and vomiting due to chemotherapy, weight gain in HIV, sleep disorders, and Tourette syndrome was low quality evidence. Cannabinoids were also associated with an increased risk of short-term adverse events such as those noted in the above quote. Future studies with large random clinical trials were said to be needed in order to confirm the effects of cannabinoids with issues such as: weight gain in patients with HIV/AIDS, depression, sleep disorders, anxiety disorders, psychosis, glaucoma, and Tourette syndrome. Additionally, the lack of research into the effects and adverse events with cannabis point to the need of future studies in these areas.
Hopefully as medical marijuana becomes more widely available in Pennsylvania, the administrators of the Medical Marijuana Program and other state policy makers will pursue the recommendations suggested in the research reviewed here by Gruber and others who are concerned that “policy has outpaced science” when it comes to lawmakers making public health decisions about recreational and medical marijuana.
Originally posted on March 6, 2018.