Pharma Problems Defy Solutions
In January 2017, President-elect Donald Trump said the pharmaceutical industry’s practices were disastrous and suggested the federal government should negotiate drug prices. He characterized the industry with getting away with murder. He said: “Pharma has a lot of lobbies, a lot of lobbyists, a lot of power. And there’s very little bidding on drugs.” The response from the industry’s top trade group, the Pharmaceutical Research and Manufacturers of America (PhRMA), was to increase its lobbying expenditures from $20 million in 2016 to $25.4 million in 2017. The biggest jump occurred in the first quarter of 2017. Only the U.S. Chamber of Commerce and the National Association of Realtors outspent PhRMA lobbying in 2017.
Writing for The Hill in January of 2018, Jessie Hellmann commented that despite the president’s tough talk, “his administration has yet to take action toward lowering drug prices, and some of his policies have even been viewed as being favorable to the industry.” Danit Felber noted the same thing in the first article of her two part series for Vision Magazine. She added how President Trump selected a former Eli Lilly executive as his Secretary of Health and Human Services. “There’s no doubt that the pharmaceutical industry is growing rapidly, as are its donations to political campaigns.”
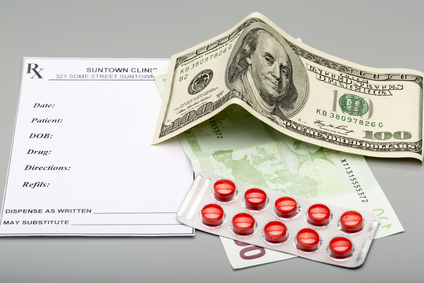
Between the years 1997 to 2016, the U.S. population grew by 21% but the number of prescriptions (to both adults and children) grew by 85%. One in every six Americans takes a psychiatric drug (antidepressants, anxiety relievers, antipsychotics, etc.) – many of the conditions treated with these drugs can be treated in whole or in part by lifestyle changes and/or therapy. And in 2014, close to 1.3 million people went to the emergency room for adverse drug effects and about 124,000 of those died (U.S. government data cited by Consumer Reports).
An infographic linked by Vision Magazine reported in 2012, 46% of American adults took prescription drugs. 11.5% of American adults take 3 or more prescription drugs; 6.5% take 4 or more. There were 4.2 billion prescriptions written in 2011—an average of 13 per average American. The amount of money spent on prescription drugs increased from $208 billion in 2001, to $234 billion in 2008, to %325 billion in 2012. Among older adults, 46% above 55 are on a prescription drug; 12.6% above 65 take 4 or more prescription drugs.
Danit Felber noted how the U.S. is only one of two countries globally that permits direct-to-consumer advertising for prescription drugs. She also pointed out that Congress passed a bill restricting the DEA from addressing the black market prescription drug trade the same way they go after the illicit drug trade. See “Head of a Snake” for more information on this. Tom Marino withdrew his name from consideration as the “drug czar” for the Trump administration when it was revealed he had spearheaded efforts to get that legislation through Congress.
The drug companies may be full of brilliant medical researchers and lawyers but it doesn’t take much brilliance to see that the American public is being exploited so pharmaceutical executives and politicians can get rich. It’s no exaggeration to say that human lives are at stake and it’s time the people understand our own place in this billion-dollar industry.
In part 2 of her series for Vision Magazine, Danit Felber reported that nine out of ten members of the U.S. House of Representatives received campaign contributions from pharmaceutical companies; as did all but three of U.S. senators. She referenced an October 2017 article in The Guardian that called out lobbying efforts of Pharma in 2016, which spent $152 million attempting to influence legislation that year; $20 million went directly to political campaigns. Reportedly, about 60% went to Republicans. Paul Ryan received $228,670. Pfizer gave $1 million towards President Trump’s inauguration.
Scores of attempts by some members of Congress to introduce legislation to bring down the price of prescription medicines or to let people buy them from Canada, where they are often cheaper, have failed to make it out of committee.
Bloomberg reported the industry’s lobbying trend continued into 2018. PhRMA spent $9.96 million on federal lobbying in the first quarter of 2018, an increase of almost $2 million from the same quarter in 2017. Several pharmaceutical companies, including Bayer Corp., AbbVie Inc, Sanofi US and Novo Nordisk all had new highs for their lobbying expenditures. PhRMA successfully stopped legislation that would have permitted generic-drug companies to study patented pharmaceutical products in order to bring low cost alternatives to market.
Bayer spent $3.45 million, AbbVie $2.89 million, Sanofi $2.03 million, Celgene $1.22 million and Novo Nordisk $1.46 million. In addition to the records, Pfizer Inc. spent $4.65 million, up from $3.79 a year earlier. Merck & Co. spent $3.31 million, nearly double its spending in the first quarter of 2017. Eli Lilly & Co. spent $1.34 million, down from $1.39 million a year earlier. Abbott Laboratories spent $790,000 in the first quarter, the same as it had in the same period in 2017.
Polls indicate high drug prices are one of Americans top health care concerns. During the 2016 presidential campaign both Hillary Clinton and Donald Trump attacked drug makers, so pharmaceutical companies stepped up their lobbying and nervously waited to see what action the President would take. One lobbyist said: “Anyone who thought the industry is fine because Hillary Clinton lost is naïve.” Companies, he thought, will want to talk with him, “particularly since his words have such an immediate impact on stock prices.”
So it was with some trepidation that Pharma faced the President’s announced plan to put “American Patients First” on May 11, 2018. In a speech given in the Rose Garden, he said: “Everyone involved in the broken system — the drug makers, insurance companies, distributors, pharmacy benefit managers and many others — contribute to the problem.” The President added that government—under previous leaders—was part of the problem by turning a blind eye to the abuse. “But under this administration we are putting American patients first.”
However, The New York Times quoted a securities analyst who said the president’s speech was “very, very positive to pharma. . . . We have not seen anything about that speech which should concern investors.” As a matter of fact,
Shares of several major drug and biotech companies rose immediately after the speech. Drugmakers’ stocks jumped immediately after the speech, as did the stocks of pharmacy benefit managers, the “middlemen” who Mr. Trump said had gotten “very, very rich.”Rather than take aim at the pharmaceutical makers, Mr. Trump said his administration would cut out the middleman, provide new tools to private benefits managers in Medicare’s prescription drug program to negotiate lower prices, stop limiting pharmacists from helping patients save money and speed up approval of over-the-counter medicines so that fewer will require prescriptions.
The Washington Post pointed out “American Patients First” suggested a number of policy ideas without a specific timeline for implementations. It excluded an idea Trump had previously proposed: “allowing the government to negotiate drug prices on behalf of the Medicare program.” It was silent about allowing Americans to import low-cost prescriptions from other countries like Canada. There was also evidence that some of the ideas spread by the pharmaceutical lobby took root. “Over the past year, drug companies have sought to deflect criticisms of their prices by blaming a secretive tier of middleman industries, such as pharmacy benefit managers that negotiate drug prices, for the role they play in prices.”
In addition to turning away from drug companies to condemn the “middleman” of PBMs—pharmacy-benefit managers—President Trump said he would make it a priority to stop foreign countries from getting drastically lower prices than in the U.S. Yet there isn’t a clear path to see that an increase in foreign prices would offset U.S. drug prices. Allan Coukell from the Pew Charitable Trusts commented: “I haven’t seen so far any manufacturers stepping forward to say how much they would lower prices in the U.S. if the U.K. and Germany paid more.” Rachel Sachs, an associate professor of law at Washington University School of Law, said: “With all the buildup the administration has given it, the president’s speech was deeply underwhelming. There is very little new in the administration’s plan, and little if anything that will make a difference in the near future, as the president has promised.” Gerard Anderson, a professor at John Hopkins Bloomberg School of Public Health, said: “He diagnosed the problems very well, and just didn’t have a solution.”