Death, Taxes and Dementia
Are you 55 or older and do you take an antidepressant or an antipsychotic medication? What about an antiepileptic drug? How about an antiparkinson or an antimuscarinic medication for an overactive bladder? These medications are probably anticholinergic drugs and if you use them regularly, you could be at a 50% higher risk of dementia. However, before looking at the evidence showing how anticholinergic medications could lead to dementia, we need to first understand a few things about these drugs.
Older adults with multiple co-occurring medical conditions are likely to be prescribed medications with anticholinergic properties, drugs that block the action of the neurotransmitter acetylcholine (Ach). These drugs are associated with many side-effects and are consistently shown to be associated with the later development of cognitive problems and dementia. Given the association between anticholinergic exposure and adverse effects, accurate quantification of anticholinergic burden (the cumulative effect over time) is needed to assess the risks versus benefits of prescribing these medications. There are a number of scales and measures that have been developed to assess anticholinergic burden.
“A review of published anticholinergic scales and measures” in Archives of Gerontology and Geriatrics found that the Anticholinergic Cognitive Burden (ACB) Scale was well suited to use in observational studies where anticholinergic exposure needed to quantified because it considered a large number of medications. The ACB Scale was developed by Malaz Boustani of the Aging Brain Program of Indiana University. Drugs were given a score of 1 if lab tests indicated possible anticholinergic effects, but there was no evidence of clinically relevant cognitive effects. A drug was given a score of 2 or 3 if it has established, clinically relevant anticholinergic effects.
A study by Coupland et al, “Anticholinergic Drug Exposure and the Risk of Dementia” concluded that regular use of some anticholinergic medications increased your risk of developing dementia by 50%. The researchers found significant increases in dementia risk for anticholinergic antidepressants, antiparkinson drugs, antipsychotics, antiepileptics, and urological/antimuscarinic drugs. According to Peter Simons, who reviewed the study for Mad in America, “The researchers estimated that 10% of all new dementia cases are due to the adverse effects of these medications.” The increased risk of dementia was projected from a total anticholinergic exposure equivalent to “3 years’ daily use of a single strong exposure medication at the minimum effective dose recommended for older people.” These findings were consistent with 3 other studies and the coherence of their findings provided strong evidence for the study’s reliability.
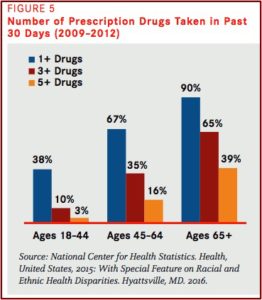
One of these studies was “Anticholinergic drugs and risk of dementia: case control study” by Richardson et al. The researchers said while middle aged and older adults are increasingly taking multiple anticholinergic drugs, the potential adverse effects of long-term use were not well understood. The researchers selected patients with a new diagnosis of dementia and compared their prescriptions of anticholinergic medications 4-20 years before the diagnosis of dementia with a matched group of patients without dementia. They found a noticeable association between an increasing anticholinergic burden over the previous 4-20 years and the occurrence of dementia. This dose-response effect was only evident for certain classes of anticholinergic drugs, antidepressants and urologicals/antimuscarinics. Significantly these relations were seen even when the drugs were used 15-20 years before the dementia diagnosis.
“The association with dementia increases with greater exposure to these types of medication,” said George Savva, who was one of the researchers. He cautioned that the study only showed an association, not a cause. “But because our research shows that the link goes back up to 15 or 20 years before someone is eventually diagnosed with early dementia symptoms, probably isn’t the case.” Fortunately, there is no apparent risk with anticholinergic drugs used to treat common conditions, like hay fever, travel sickness and stomach cramps. “The risk of dementia increased with greater exposure for antidepressant, urological, and antiparkinson drugs with an ACB score of 3.”
Although Richardson et al did not find the risk of dementia increased with exposure to antipsychotics, it should be noted that several antipsychotics, including Thorazine, Zyprexa, Trilafon, Seroquel, Mellaril, and Stelazine have an ACB score of 3. The antidepressants amitriptyline (Elavil) and paroxetine (Paxil) have an ACB score of 3 and were among the five most commonly prescribed drugs in the study. Less popular antidepressants with an ACB score of 3 included Anafranil, Tofranil, Sinequan, and Surmontil. Antidepressants with an ACB scores of 1 (Wellbutrin, Luvox, Effexor, Trazodone), were associated with dementia, but the association was greater when these antidepressant prescriptions were given close to the timing of the dementia diagnosis. Abilify, an antidepressant and Effexor, an antidepressant, were given a score of 1 in a 2012 update to the ACB Scale.
The organization Health in Aging Foundation, created by the American Geriatrics Society, adds some additional medications that older adults should be wary of. There is a helpful Tip Sheet on its HealthinAging.org website, “Ten Medications Older Adults Should Avoid or Use With Caution.” The noted medications expand the adverse side effects for older adults from certain medications beyond just the risks for cognitive decline and dementia. They also underscore some of the warnings given above. For instance, the caution against antipsychotics was in bold: “If you are NOT being treated for psychosis, use antipsychotics WITH CAUTION.” Antipsychotics are commonly used to treat behavioral problems in older adults with dementia, where they increase the risk of stroke and even death.
Avoiding medications for anxiety (such as benzodiazepines) or insomnia such as Sonata (zaleplon), Ambien (zolpidem) and Lunesta (eszopiclone) was suggested. These drugs increase the risk of falls and can cause confusion. “Because it takes your body a long time to get rid of these drugs, these effects can carry into the day after you take the medication.” Muscle relaxants such as Flexeril (cyclobenzaprine; ACB score of 2), Robaxin (methocarbamol, ACB score of 3) and Soma (carisoprodol) can leave you feeling groggy and increase your risk of falls as well. “Plus, there is little evidence that they work well.” Women should avoid estrogen pills and patches prescribed for hot flashes and other menopause-related symptoms, as they can increase the risk of breast cancer and blood clots.
Psychiatric Times published a literature review, “Benzodiazepine Use and the Risk of Dementia,” that evaluated the evidence benzodiazepine use may increase the risk of dementia in older adults. They found 15 studies that assessed the association between benzodiazepine use and the development of dementia. Of the 15 studies, 8 showed a positive association between benzodiazepine use and dementia. The authors said given the prevalence of benzodiazepine use among older adults, the association between benzodiazepines and the development of dementia is a major cause of concern.
A study among older adults in the province of Quebec, Canada published in the BMJ, “Benzodiazepine use and risk of Alzheimer’s disease: case-control study,” found that benzodiazepine use was associated with an increased risk of Alzheimer’s disease. “The risk of Alzheimer’s disease was increased by 43-51% among those who had used benzodiazepines in the past.” There was a dose-effect relationship between benzodiazepine use and increased risk of Alzheimer’s disease in older people treated previously for more than three months. There was also a higher risk with long-acting formulas.
These medication concerns overlap an existing and growing problem as Americans grow older. In the United States, the number of Americans 65 and older was projected to nearly double from 53 million in 2018 to 95 million by 2060. That age group’s share of the total population is supposed to rise from 16% to 23%. The aging baby boomer generation may also fuel a 50% increase in the number of Americans requiring nursing home care. “Demand for elder care will also be driven by a steep rise in the number of Americans living with Alzheimer’s disease, which could more than double by 2050 to 13.8 million, from 5.8 million today.” So, an increase of older adults living with Alzheimer’s disease (not counting those with dementia) of over 200% is expected by 2050.
The word at this point seems to be that the influence of anticholinergic medications on the rates of dementia in older adults cannot be proven with certainty. Yet the evidence suggests there is a relationship. Maybe by 2050 we will have found a cure for dementia and Alzheimer’s; maybe not. However, there was a Dutch study suggesting that dementia and Alzheimer’s disease may not be an inevitable part of aging. Dr. Richard Isaacson, the director of the Alzheimer’s Prevention Clinic at Weill Cornell Medicine and New York-Presbyterian Hospital told ABC News that dementia and Alzheimer’s tend to have multifactorial conditions. This means “that a mix of genetics, age, environment, lifestyle behaviors and medical conditions that coexist together and can lead a person toward or away from cognitive decline.”
The takeaway seems to be we can be certain of cognitive decline from dementia or Alzheimer’s with older adults, but we can’t be certain of what causes it. Benjamin Franklin said, “in this world nothing can be said to be certain, except death and taxes.” Perhaps we can suggest in this world nothing can be certain except death, taxes and dementia.