The Brute Facts of Depression Genetics
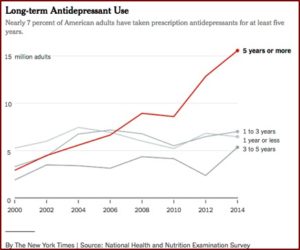
1996 was in the midst of the golden years for associating serotonin and depression. SSRIs like fluoxetine (Prozac, 1987), sertraline (Zoloft, 1991), paroxetine (Paxil, 1992) and fluvoxamine (Luvox, 1994) were on the market. Citalopram (Celexa, 1998) and escitalopram (Lexapro, 2002) would join them over the next six years. A study was published in 1996 claiming to have identified a gene, 5-HTTLPR, that was a “potential genetic susceptibility factor for affective disorders” like depression. The chemical imbalance or serotonin imbalance theory of depression was a self-evident fact, promoted by the pharmaceutical companies in their consumer advertisements, like this one for Prozac:
When you’re clinically depressed, one thing that can happen is the level of serotonin (a chemical in your body) may drop. So you may have trouble sleeping. Feel unusually sad or irritable. Find it hard to concentrate. Lose your appetite. Lack energy. Or have trouble feeling pleasure…to help bring serotonin levels closer to normal, the medicine doctors now prescribe most often is Prozac®.
But with the growth and acceptance of critiques of the chemical imbalance theory like those of Lacasse and Leo in “Antidepressants and the Chemical Imbalance Theory of Depression: “The number of websites making such claims dropped, with some websites going dark or minimalist as the drug patent ran out.” Newer medications altered their rhetoric to say they were “adjusting” or “affecting” neurotransmitter levels instead of “correcting a chemical imbalance.” Psychiatrists like Ronald Pies distanced themselves from the chemical imbalance theory, saying it was “always a kind of urban legend,” but never a theory that well-informed psychiatrists believed. It was simply “a little white lie,” according to Dr. Pies. (editor’s note: it is more correct to say Lacasse and Leo said Dr. Pies said it was simply “a little white lie.” More on this later.) Lacasse and Leo further noted: “We can’t help but notice that the silence of psychiatry regarding chemical imbalance only ended when the profits had been extracted from the SSRI marketplace.”
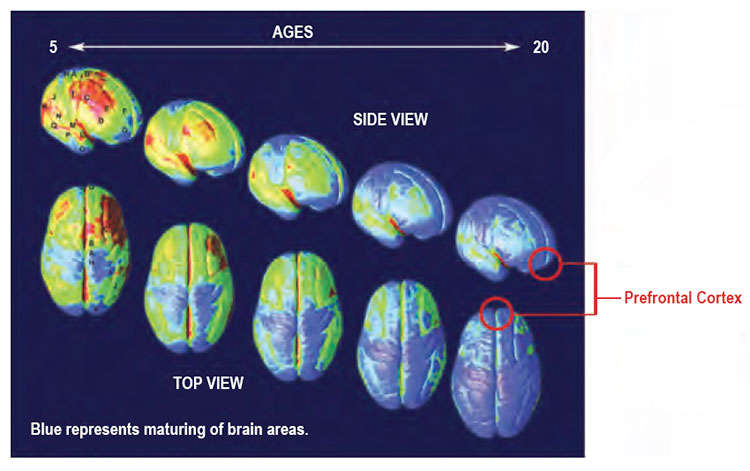
But interest in the 5-HTT gene persisted. In 2003 Caspi et al. published a paper on the influence of life stress on depression moderated by the 5-HTT serotonin transporter. Then, as noted by Scott Alexander in his blog, “5-HTTLPR was found to directly affect the reactivity of the HPA axis, the stress processing circuit leading from the adrenal glands to the brain.” Studies began to show an association with other psychiatric disorders such as seasonal affective disorder, insomnia, anxiety, even psychosis. Researchers began to suspect that genes like 5-HTTLPR may also moderate how we respond to life events.
A meta-analysis looked at 54 studies of the interaction and found “strong evidence that 5-HTTLPR moderates the relationship between stress and depression, with the s allele associated with an increased risk of developing depression under stress (P = .00002)”. This relationship was then independently re-confirmed for every conceivable population and form of stress. Depressed children undergoing childhood adversity. Depressed children with depressed mothers. Depressed youth. Depressed adolescent girls undergoing peer victimization. They all developed different amounts of depression based on their 5-HTTLPR genotype.
There were studies on how 5-HTTLPR and stress interacted with gender, parenting, decision-making, single motherhood and more. There were also studies of its relevance in antidepressant treatment, specifically with citalopram and fluvoxamine. “A meta-analysis of 15 studies found that 5-HTTLPR genotype really did affect SSRI efficacy (p = 0.0001).” Psychiatrists were urged to test for 5-HTTLPR before treating patients. However, as Dr. Alexander concluded after reading Border et al.’s study: “ALL OF THIS IS LIES.”
The authors said that given what we now know about polygenicity, studies of individual single-nucleotide polymorphism (SNP) like Caspi et al. does with the 5-HTTLPR gene require samples of around 34,000 people to detect an effect. “So any study with fewer than 34,000 people that says anything about specific genes is almost definitely a false positive.” The median size for the above discussed studies was 345.
We examined multiple types of associations between18 highly studied candidate genes for depression and multiple depression phenotypes. The study was very well powered compared with previous candidate gene studies, with Ns ranging from 62,138 to 443,264 across subsamples. Despite the high statistical power, none of the most highly studied polymorphisms within these genes demonstrated substantial contributions to depression liability. Furthermore, we found no evidence to support moderation of polymorphism effects by exposure to traumatic events or socioeconomic adversity.
Attempting to be fair to the psychiatric research community, Alexander said over the past fifteen years many people have voiced concerns with 5-HTTLRP findings. One study that failed to replicate findings was published in 2009. Risch et al. concluded “This meta-analysis yielded no evidence that the serotonin transporter genotype alone or in interaction with stressful life events is associated with an elevated risk of depression in men alone, women alone, or in both sexes combined.” Alexander further said that Border et al. did not prove every single 5-HTTLPR study was wrong. However, it did cast doubt upon them.
The authors of this paper are geneticists who are politely trying to explain how genetics works to psychiatrists. They are arguing that single genes usually matter less than people think. They do an analysis of depression to demonstrate that they know what they’re talking about, but the points they are making apply to insomnia, nostalgia, and everything else. So all the studies above are at least questionable.
Before placing this in an “anti-psychiatry” box and dismissing it, consider the implications of how this happened. This was shoddy science, plain and simple. And “since crappy science will find whatever it’s looking for—it was appropriately discovered that yes, changes in the serotonin transporter gene caused depression.” Alexander said the magnitude of the problem is not just a minor difference in methodology along the lines of sometimes failing to get an effect in a cold room, when the original study occurred in a hot room. It is more like “you can get an entire field with hundreds of studies analyzing the behavior of something that doesn’t exist.”
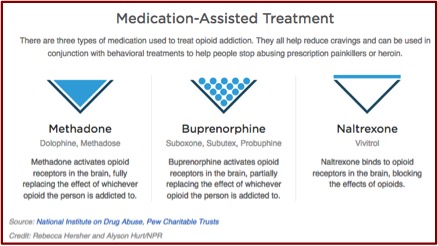
Another issue is the implications the findings have for antidepressant pharmacogenomic testing. Remember the reference to studies on 5-HTTLPR and antidepressant treatment? Assuming their validity, your psychiatrist could order a genetic test to see which antidepressant is right for you. These tests have become part of care in some hospitals, they’ve insinuated themselves into psychiatry residency programs; they’ve become part of high-priced concierge medical systems. GeneSight, one of the most popular tests, uses seven genes—one of which contains the 5-HTTLPR as a subregion. “But since the only reason we thought that they might [work] was because of evidence they affected depression, and now it seems they don’t affect depression, it’s less likely that they affect antidepressant response too.”
Remember, GeneSight and their competitors refuse to release the proprietary algorithms they use to make predictions. They refuse to let any independent researchers study whether their technique works. They dismiss all the independent scientists saying that their claims are impossible by arguing that they’re light-years ahead of mainstream science and can do things that nobody else can. If you believed them before, you should be more cautious now. They are not light-years ahead of mainstream science. They took some genes that mainstream science had made a fuss over and claimed they could use them to predict depression. Now we think they were wrong about those. What are the chances they’re right about the others? Yes, GeneSight has ten or twenty studies proving that their methods work. Those were all done by scientists working for GeneSight. Remember, if you have bad science you can prove whatever you want.
Even in science, there is no such thing as a brute, uninterpreted fact.
********
(Revised on 7/28/2019)
There has been an ongoing dispute since the original Lacasse and Leo article linked above over what Dr. Pies said in his article for Medscape, “Nuances, Narratives, and the ‘Chemical Imbalance Debate in Psychiatry.” Apparently, the original article did use the phrase ‘little white lie,’ but was revised after others took note of Dr. Pies’ use of the phrase. According to Philip Hickey, PhD who was writing for Mad in America, the third paragraph of the article originally read:
“Now, if you were to give credence to a recent online polemic posing as investigative journalism, you would probably choose the first or second statement. In the narrative of the antipsychiatry movement, a monolithic entity called ‘Psychiatry’ has deliberately misled the public as to the causes of mental illness, by failing to debunk the chemical imbalance hypothesis. Indeed, this narrative insists that, by promoting this little white lie, psychiatry betrayed the public trust and made it seem as if psychiatrists had magic bullets for psychiatric disorders. (Lurking in the back-story, of course, is Big Pharma, said to be in cahoots with Psychiatry so as to sell more drugs).”
The article now has “simplistic formulation” instead of ‘little white lie.’ Dr. Pies did acknowledge he failed to put the phrase ‘little white lie’ in quotes and took responsibility for the omission (See his letter to the editor, “Response to Lacasse and Leo” attached with the above-linked article by Lacasse and Leo: “Antidepressants and the Chemical Imbalance Theory of Depression”). Dr. Pies did say in his letter:
I would regard such a statement [“Your emotional problem is due to simply to a chemical imbalance”] as simplistic and reductionistic, and would never shrug it off—as Lacasse and Leo imply—as “a little white lie.” Lacasse and Leo may have made an innocent mistake in attributing this expression to me, owing to two online versions of my “Nuances” article (2014a, 2014b).
Dr. Pies further said the American Psychiatric Association’s 1978 “Position Statement on Active Treatment” declared, “Psychiatric disorders result from the complex interaction of physical, psychological, and social factors and treatment may be directed toward any or all three of these areas.” He concluded this was precisely what he and most of his academic colleagues have been teaching for the last thirty years. However, Philip Hickey addressed the nuances of this dispute in his article linked above and then summarized his conclusions on the ‘little white lie’ issue as follows:
So, to summarize the “little white lie” issue:
- In the original Psychiatric Times and Medscape articles, Dr. Pies characterized the spurious chemical imbalance theory as “this little while lie”. There was nothing in the wording of this statement to suggest that this was anything other than his own position.
- At some point in the next few weeks [Dr. Hickey’s article was dated November 17, 2015], Dr. Pies realized that his statement was inaccurate, or that he had misexpressed himself, and made an appropriate correction in the Psychiatric Times article, but not in the Medscape piece.
- In October 2015, Drs. Lacasse and Leo, accurately and appropriately, attributed the “little white lie” phrase in the Medscape article to Dr. Pies.
- Sometime in the last two weeks, the Medscape article was amended to read “simplistic formulation”.
- On November 4, 2015, Dr. Pies unjustly accused Drs. Lacasse and Leo of misattributing the phrase to him.
Dr. Pies read my article and expressed concern (see the Disqus comments below) that what I said above was erronous: “It was simply ‘a little white lie,’ according to Dr. Pies.” As the above additions to this article show, he seems to have unintentionally implied it in his original Medscape article which read, “by promoting this little white lie, psychiatry betrayed the public trust and made it seem as if psychiatrists had magic bullets for psychiatric disorders.” The revision of little white lie with simplistic formulation is clearer without leading to the misquoting of Dr. Pies that Lacasse and Leo, and me following their lead, made. Drs. Lacasse and Leo in their “Response to Daniel Carlat (2015) and Ronald Pies (2015)” said they accept Dr. Pies and his statement that he does not endorse calling the chemical imbalance theory a “little white lie” and appreciate his acknowledgement of making an editorial error. I do as well and appreciate his bringing it to my attention.
Dr. Pies went on to refer to a recent article he wrote on April 30, 2019 for Psychiatric Times, “Debunking the Two Chemical Imbalance Myths, Again.” Coincidentally, Philip Hickey published a critique of that article on Mad in America, “The Chemical Imbalance Theory: Dr. Pies Returns, Again” on July 22, 2019, the day before my article here was scheduled to be published, July 23, 2019. The two myths that Dr. Pies debunked were 1) psychiatric disorders in general are caused by a “chemical imbalance” in the brain; and 2) that “Psychiatry” as a profession endorsed the first myth, deliberately and knowingly lying to countless, unsuspecting patients.
See the two articles for more specific details. But clearly, the dispute over whether or not psychiatry (lower case “p”) as a profession endorsed the chemical imbalance myth is still a valid critique, and not simply a myth. Dr. Hickey noted the American Psychiatric Association published a 2005 brochure called “Let’s Talk Facts About Depression.” It is apparently no longer available on the APA website, but is available other places by searching for the title. The link here is to a copy Dr. Hickey placed on the Mad in America website. The brochure does say several factors play a role in the onset of depression, biochemistry, genetics, personality and environmental factors. Yet under the biochemistry factor it states,
Abnormalities in two chemicals in the brain, serotonin and norepinephrine, might contribute to symptoms of depression, including anxiety, irritability and fatigue. Other brain networks undoubtedly are involved as well; scientists are actively seeking new knowledge in this area.
And in response to the question, “How Is Depression Treated?,” under Medication it states, “Antidepressants may be prescribed to correct imbalances in the levels of chemicals in the brain.” These statements were published fourteen years ago, long before the current dispute. But they illustrate how at least one of the two chemical imbalance “myths” of Dr. Pies is not quite as debunked as he thinks it should be. And there is perhaps a clarification needed in his “Debunking” article, where he initially says “The first [myth] holds that mental illnesses (psychiatric disorders) in general are caused by ‘a chemical imbalance’ in the brain—the so-called “chemical imbalance theory” (CIT).” Then two paragraphs later seems to expand the myth to mean belief in a GUT, grand unified theory of mental illness in general: “Scientifically speaking, there never was a network of validated hypotheses capable of sustaining a full-blown, global ‘chemical imbalance theory’ of mental illness in general.”
I think it is worth repeating here that even in science, there is no such thing as a brute, uninterpreted fact. Here I am thinking of a ‘brute fact’ consistent with how Cornelius Van Til, a theologian understands it. See “The Limits of Human Reason” for more on this.